Fibroblast growth factor receptor 3
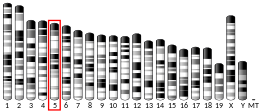
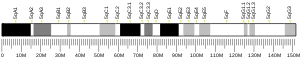
Fibroblast growth factor receptor 3 is a protein that in humans is encoded by the FGFR3 gene.[5] FGFR3 has also been designated as CD333 (cluster of differentiation 333). The gene, which is located on chromosome 4, location p16.3, is expressed in tissues such as the cartilage, brain, intestine, and kidneys.[6]
The FGFR3 gene produces various forms of the FGFR3 protein; the location varies depending on the isoform of the FGFR3 protein. Since the different forms are found within different tissues the protein is responsible for multiple growth factor interactions.[7] Gain of function mutations in FGFR3 inhibits chondrocyte proliferation and underlies achondroplasia and hypochondroplasia.
Function[edit]
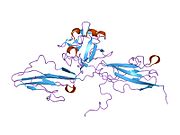
The protein encoded by this gene is a member of the fibroblast growth factor receptor family, where amino acid sequence is highly conserved between members and throughout evolution. FGFR family members differ from one another in their ligand affinities and tissue distribution. A full-length representative protein would consist of an extracellular region, composed of three immunoglobulin-like domains, a single hydrophobic membrane-spanning segment and a cytoplasmic tyrosine kinase domain. The extracellular portion of the protein interacts with fibroblast growth factors, setting in motion a cascade of downstream signals which ultimately influence cell mitogenesis and differentiation.
This particular family member binds both acidic and basic fibroblast growth factor and plays a role in bone development and maintenance. The FGFR3 protein plays a role in bone growth by regulating ossification.[7] Alternative splicing occurs and additional variants have been described, including those utilizing alternate exon 8 rather than 9, but their full-length nature has not been determined.[8]
Mutations[edit]
Simplification on the mutation 46 XX 4q16.3 (female), 46XY 4q16.3 (male). Gain of function mutations in this gene can develop dysfunctional proteins "impede cartilage growth and development and affect chondrocyte proliferation and calcification"[6] which can lead to craniosynostosis and multiple types of skeletal dysplasia (osteochondrodysplasia).
In achondroplasia, the FGFR3 gene has a missense mutation at nucleotide 1138 resulting from either a G>A or G>C.[9] This point mutation in the FGFR3 gene causes hydrogen bonds to form between two arginine side chains leading to ligand-independent stabilization of FGFR3 dimers. Overactivity of FGFR3 inhibits chondrocyte proliferation and restricts long bone length.[7]
FGFR3 mutations are also linked with spermatocytic tumor, which occur more frequently in older men.[10]
Disease linkage[edit]
Defects in the FGFR3 gene has been associated with several conditions, including craniosynostosis and seborrheic keratosis.[11]
Bladder cancer[edit]
Mutations of FGFR3, FGFR3–TACC3 and FGFR3–BAIAP2L1 fusion proteins are frequently associated with bladder cancer, while some FGFR3 mutations are also associated with a better prognosis. Hence FGFR3 represents a potential therapeutic target for the treatment of bladder cancer.[12]
Post-translational modification of FGFR3 occur in bladder cancer that do not occur in normal cells and can be targeted by immunotherapeutic antibodies.[13]
Glioblastoma[edit]
FGFR3-TACC3 fusions have been identified as the primary mitogenic drivers in a subset of glioblastomas (approximately 4%) and other gliomas and may be associated with slightly improved overall survival.[14] The FGFR3-TACC3 fusion represents a possible therapeutic target in glioblastoma.
Achondroplasia[edit]
Achondroplasia is a dominant genetic disorder caused by mutations in FGFR3 that make the resulting protein overactive. Individuals with these mutation have a head size that is larger than normal and are significantly shorter in height.[15][16] Only a single copy of the mutated FGFR3 gene results in achondroplasia.[17] It is generally caused by spontaneous mutations in germ cells; roughly 80 percent of the time, parents with children that have this disorder are normal size.[16][17]
Thanatophoric dysplasia[edit]
Thanatophoric dysplasia is a genetic disorder caused by gain-of-function mutations in FGFR3 that is often fatal during the perinatal period because the child cannot breathe.[18][19] There are two types. TD type I is caused by a stop codon mutation that is located in part of the gene coding for the extracellular domain of the protein.[18] TD type II is a result of a substitution in a Lsy650Glu which is located in the tyrosine kinase area of FGFR3.[18]
Muenke syndrome[edit]
Muenke syndrome, a disorder characterized by craniosynostosis, is caused by protein changes on FGFR3. The specific pathogenic variant c.749C>G changes the protein p.Pro250Arg, in turn resulting in this condition.[20] Characteristics of Muenke syndrome include coronal synostosis (usually bilateral), midfacial retrusion, strabismus, hearing loss, and developmental delay. Turribrachycephaly, cloverleaf skull, and frontal bossing are also possible.[21]
As a drug target[edit]
FGFR3 inhibitors are in early clinical trials as a cancer treatment,[citation needed] e.g. BGJ398 for urothelial carcinoma.[22] The FGFR3 receptor has a tyrosine kinase signaling pathway that is associated with many biological developments embryonically and in tissues.[citation needed] Studying the tyrosine kinase signaling pathway that FGFR3 displays has played a crucial role in the development of research of several cell activities such as cell proliferation and cellular resistance to anti-cancer medications.[citation needed]
Interactions[edit]
Fibroblast growth factor receptor 3 has been shown to interact with FGF8[23][24] and FGF9.[23][24]
See also[edit]
References[edit]
- ^ a b c GRCh38: Ensembl release 89: ENSG00000068078 – Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000054252 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ Keegan K, Johnson DE, Williams LT, Hayman MJ (February 1991). "Isolation of an additional member of the fibroblast growth factor receptor family, FGFR-3". Proceedings of the National Academy of Sciences of the United States of America. 88 (4): 1095–9. Bibcode:1991PNAS...88.1095K. doi:10.1073/pnas.88.4.1095. PMC 50963. PMID 1847508.
- ^ a b Wang Y, Liu Z, Liu Z, Zhao H, Zhou X, Cui Y, Han J (May 2013). "Advances in research on and diagnosis and treatment of achondroplasia in China". Intractable & Rare Diseases Research. 2 (2): 45–50. doi:10.5582/irdr.2013.v2.2.45. PMC 4204580. PMID 25343101.
- ^ a b c "FGFR3 gene". Genetics Home Reference. U.S. National Library of Medicine. Retrieved 2018-09-27.
- ^ "Entrez Gene: FGFR3 fibroblast growth factor receptor 3 (achondroplasia, thanatophoric dwarfism)".
- ^ Foldynova-Trantirkova S, Wilcox WR, Krejci P (January 2012). "Sixteen years and counting: the current understanding of fibroblast growth factor receptor 3 (FGFR3) signaling in skeletal dysplasias". Human Mutation. 33 (1): 29–41. doi:10.1002/humu.21636. PMC 3240715. PMID 22045636.
- ^ Kelleher FC, O'Sullivan H, Smyth E, McDermott R, Viterbo A (October 2013). "Fibroblast growth factor receptors, developmental corruption and malignant disease". Carcinogenesis. 34 (10): 2198–205. doi:10.1093/carcin/bgt254. PMID 23880303.
- ^ Hafner C, Hartmann A, Vogt T (July 2007). "FGFR3 mutations in epidermal nevi and seborrheic keratoses: lessons from urothelium and skin". The Journal of Investigative Dermatology. 127 (7): 1572–3. doi:10.1038/sj.jid.5700772. PMID 17568799.
- ^ di Martino E, Tomlinson DC, Williams SV, Knowles MA (October 2016). "A place for precision medicine in bladder cancer: targeting the FGFRs". Future Oncology (London, England). 12 (19): 2243–63. doi:10.2217/fon-2016-0042. PMC 5066128. PMID 27381494.
- ^ Oo HZ, Seiler R, Black PC, Daugaard M (October 2018). "Post-translational modifications in bladder cancer: Expanding the tumor target repertoire". Urologic Oncology. 38 (12): 858–866. doi:10.1016/j.urolonc.2018.09.001. PMID 30342880. S2CID 53041768.
- ^ Mata, Douglas A.; Benhamida, Jamal K.; Lin, Andrew L.; Vanderbilt, Chad M.; Yang, Soo-Ryum; Villafania, Liliana B.; Ferguson, Donna C.; Jonsson, Philip; Miller, Alexandra M.; Tabar, Viviane; Brennan, Cameron W.; Moss, Nelson S.; Sill, Martin; Benayed, Ryma; Mellinghoff, Ingo K.; Rosenblum, Marc K.; Arcila, Maria E.; Ladanyi, Marc; Bale, Tejus A. (2020). "Genetic and epigenetic landscape of IDH-wildtype glioblastomas with FGFR3-TACC3 fusions". Acta Neuropathologica Communications. 8 (1): 186. doi:10.1186/s40478-020-01058-6. PMC 7653727. PMID 33168106.
- ^ "Achondroplasia". Genetic and Rare Diseases Information Center (GARD).
- ^ a b "FGFR3 gene". Genetics Home Reference. U.S. National Library of Medicine.
- ^ a b "Learning about Achondroplasia". National Human Genome Research Institute. Retrieved July 15, 2016.
- ^ a b c Karczeski B, Cutting GR (1993). Adam MP, Ardinger HH, Pagon RA, Wallace SE, Bean LJ, Stephens K, Amemiya A (eds.). Thanatophoric Dysplasia. University of Washington, Seattle. PMID 20301540. Retrieved 2018-11-17.
{{cite book}}:|work=ignored (help) - ^ Nissenbaum M, Chung SM, Rosenberg HK, Buck BE (August 1977). "Thanatophoric dwarfism. Two case reports and survey of the literature". Clinical Pediatrics. 16 (8): 690–7. doi:10.1177/000992287701600803. PMID 872478. S2CID 30837380.
- ^ "Muenke syndrome (Concept Id: C1864436)". MedGen. NCBI. Retrieved March 18, 2023.
- ^ "Orphanet: Muenke syndrome". Orphanet. Retrieved March 18, 2023.
- ^ Pal SK, Rosenberg JE, Hoffman-Censits JH, Berger R, Quinn DI, Galsky MD, Wolf J, Dittrich C, Keam B, Delord JP, Schellens JH, Gravis G, Medioni J, Maroto P, Sriuranpong V, Charoentum C, Burris HA, Grünwald V, Petrylak D, Vaishampayan U, Gez E, De Giorgi U, Lee JL, Voortman J, Gupta S, Sharma S, Mortazavi A, Vaughn DJ, Isaacs R, Parker K, Chen X, Yu K, Porter D, Graus Porta D, Bajorin DF (July 2018). "FGFR3 Alterations". Cancer Discovery. 8 (7): 812–821. doi:10.1158/2159-8290.CD-18-0229. PMC 6716598. PMID 29848605.
- James Nam (May 31, 2018). "Novel FGFR3 Inhibitor May Be a New Treatment Option for Metastatic Urothelial Carcinoma". Cancer Therapy Advisor.
- ^ a b Santos-Ocampo S, Colvin JS, Chellaiah A, Ornitz DM (January 1996). "Expression and biological activity of mouse fibroblast growth factor-9". The Journal of Biological Chemistry. 271 (3): 1726–31. doi:10.1074/jbc.271.3.1726. PMID 8576175.
- ^ a b Chellaiah A, Yuan W, Chellaiah M, Ornitz DM (December 1999). "Mapping ligand binding domains in chimeric fibroblast growth factor receptor molecules. Multiple regions determine ligand binding specificity". The Journal of Biological Chemistry. 274 (49): 34785–94. doi:10.1074/jbc.274.49.34785. PMID 10574949.
Further reading[edit]
- Duperret EK, Oh SJ, McNeal A, Prouty SM, Ridky TW (2014). "Activating FGFR3 mutations cause mild hyperplasia in human skin, but are insufficient to drive benign or malignant skin tumors". Cell Cycle. 13 (10): 1551–9. doi:10.4161/cc.28492. PMC 4050160. PMID 24626198.
- Schweitzer DN, Graham JM, Lachman RS, Jabs EW, Okajima K, Przylepa KA, Shanske A, Chen K, Neidich JA, Wilcox WR (January 2001). "Subtle radiographic findings of achondroplasia in patients with Crouzon syndrome with acanthosis nigricans due to an Ala391Glu substitution in FGFR3". American Journal of Medical Genetics. 98 (1): 75–91. doi:10.1002/1096-8628(20010101)98:1<75::AID-AJMG1010>3.0.CO;2-6. PMID 11426459.
- Horton WA, Lunstrum GP (December 2002). "Fibroblast growth factor receptor 3 mutations in achondroplasia and related forms of dwarfism". Reviews in Endocrine & Metabolic Disorders. 3 (4): 381–5. doi:10.1023/A:1020914026829. PMID 12424440. S2CID 7425804.
- Bonaventure J, Silve C (November 2005). "[Hereditary skeletal dysplasias and FGFR3 and PTHR1 signaling pathways]". Médecine/Sciences. 21 (11): 954–61. doi:10.1051/medsci/20052111954. PMID 16274647.
- Hernández S, Toll A, Baselga E, Ribé A, Azua-Romeo J, Pujol RM, Real FX (July 2007). "Fibroblast growth factor receptor 3 mutations in epidermal nevi and associated low grade bladder tumors". The Journal of Investigative Dermatology. 127 (7): 1664–6. doi:10.1038/sj.jid.5700705. PMID 17255960.
- Olsen SK, Ibrahimi OA, Raucci A, Zhang F, Eliseenkova AV, Yayon A, Basilico C, Linhardt RJ, Schlessinger J, Mohammadi M (January 2004). "Insights into the molecular basis for fibroblast growth factor receptor autoinhibition and ligand-binding promiscuity". Proceedings of the National Academy of Sciences of the United States of America. 101 (4): 935–40. Bibcode:2004PNAS..101..935O. doi:10.1073/pnas.0307287101. PMC 327120. PMID 14732692.
External links[edit]
- GeneReviews/NIH/NCBI/UW entry on FGFR-Related Craniosynostosis Syndromes
- GeneReviews/NIH/NCBI/UW entry on Muenke Syndrome
- GeneReviews/NIH/NCBI/UW entry on Hypochondroplasia
- FGFR3+protein,+human at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
- Overview of all the structural information available in the PDB for UniProt: P22607 (Fibroblast growth factor receptor 3) at the PDBe-KB.
This article incorporates text from the United States National Library of Medicine, which is in the public domain.