Melatonin as a medication and supplement
Melatonin is a naturally occurring hormone produced in the brain that is also used as a dietary supplement and medication.[9][12] As a hormone, melatonin is released by the pineal gland and is involved in sleep–wake cycles.[9][12] As a supplement, it is often used for the attempted short-term treatment of disrupted sleep patterns, such as from jet lag or shift work, and is typically taken orally.[13][14][15] There is evidence of its benefit for this use, but is not strong.[16] A 2017 review found that sleep onset occurred six minutes faster with use, but found no change in total time asleep.[14]
Side effects from melatonin supplements are minimal at low doses for short durations (the studies reported about equally for both melatonin and placebo).[9][17] Side effects of melatonin are rare but may occur in 1 to 10 patients in 1,000.[17][8] They may include somnolence, headaches, nausea, diarrhea, abnormal dreams, irritability, restlessness, insomnia, anxiety, migraine, lethargy, hyperactivity, dizziness, hypertension, abdominal pain, heartburn, mouth ulcers, dry mouth, hyperbilirubinaemia, dermatitis, night sweats, pruritus, rash, dry skin, pain in the extremities, symptoms of menopause, chest pain, glycosuria (sugar in the urine), proteinuria (protein in the urine), abnormal liver function tests, weight gain, mood swings, aggression, and grogginess after awakening.[8][18][17][19][20] Its use is not recommended during pregnancy or breastfeeding or for those with liver disease.[15][20]
Melatonin acts as an agonist of the melatonin MT1 and MT2 receptors, the biological targets of endogenous melatonin.[21] It is thought to activate these receptors in the suprachiasmatic nucleus of the hypothalamus in the brain to regulate the circadian clock and sleep–wake cycles.[21] Immediate-release melatonin has a short elimination half-life of about 20 to 50 minutes.[22][9][10] Prolonged-release melatonin used as a medication has a half-life of 3.5 to 4 hours.[11][8]
Melatonin was discovered in 1958.[9] It is sold over-the-counter in Canada and the United States;[17][19] in the United Kingdom, it is a prescription-only medication.[15] In Australia and the European Union, it is indicated for difficulty sleeping in people over the age of 54.[23][8] In the European Union, it is indicated for the treatment of insomnia in children and adolescents.[18] The U.S. Food and Drug Administration (FDA) treats melatonin as a dietary supplement and, as such, has not approved it for any medical uses.[17] It was approved for medical use in the European Union in 2007.[8] Besides melatonin, certain synthetic melatonin receptor agonists like ramelteon, tasimelteon, and agomelatine are also used in medicine.[24][25] In 2021, it was the 257th most commonly prescribed medication in the United States, with more than one million prescriptions.[26][27]
Medical uses
[edit]Insomnia
[edit]There is no good evidence that melatonin helps treat insomnia and its attempted use for this purpose is recommended against by the American Academy of Sleep Medicine.[28]
A prolonged-release form of melatonin is approved for use as a medication in Europe for the treatment of insomnia in certain people.[11][29]
Circadian rhythm sleep disorders
[edit]Melatonin may be useful in the treatment of delayed sleep phase syndrome.[9]
Melatonin is known to reduce jet lag, especially in eastward travel. However, if it is not taken at the correct time, it can instead delay adaptation.[30]
Melatonin appears to have limited use against the sleep problems of people who work shift work.[31] Tentative evidence suggests that it increases the length of time people are able to sleep.[31]
REM sleep behavior disorder
[edit]Melatonin is a safer alternative than clonazepam in the treatment of REM sleep behavior disorder – a condition associated with the synucleinopathies like Parkinson's disease and dementia with Lewy bodies.[32][33][34] However, clonazepam may be more effective.[35] In any case, the quality of evidence for both treatments is very low and it is unclear whether either is definitely effective.[35]
Dementia
[edit]A 2020 Cochrane review found no evidence that melatonin helped sleep problems in people with moderate to severe dementia due to Alzheimer's disease.[36] A 2019 review found that while melatonin may improve sleep in minimal cognitive impairment, after the onset of Alzheimer's disease it has little to no effect.[37] Melatonin may, however, help with sundowning (increased confusion and restlessness at night) in people with dementia.[38]
Available forms
[edit]
A prolonged-release 2 mg oral formulation of melatonin sold under the brand name Circadin is approved for use in the European Union in the short-term treatment of insomnia in people age 55 and older.[11][29][8]
Melatonin is also available as an over-the-counter dietary supplement in many countries. It is available in both immediate-release and less commonly prolonged-release forms. The compound is available in supplements at doses ranging from 0.3 mg to 10 mg or more. It is also possible to buy raw melatonin powder by the weight.[39] Immediate-release formulations of melatonin cause blood levels of melatonin to reach their peak in about an hour. The hormone may be administered orally, as capsules, gummies, tablets, oral films, or liquids.[40] It is also available for use sublingually, or as transdermal patches.[41] Several inhalation-based melatonin products with a wide range of doses are being sold but the safety remains to be evaluated.[40]
The American Academy of Sleep Medicine (AASM) said that the melatonin content in unregulated (without a USP verified mark) supplements can diverge widely from the claimed amount; a study found that the melatonin content ranged from one half to four times the stated dose.[42]
Contraindications
[edit]Contraindications of melatonin include hypersensitivity reactions among others.[8] It is not recommended in people with autoimmune diseases due to lack of data in these individuals.[8] Prolonged-release pharmaceutical melatonin (Circadin) contains lactose and should not be used in people with the lactase deficiency or glucose–galactose malabsorption.[8] Use of melatonin is also not recommend in women who are pregnant or breastfeeding or in people with liver disease.[15][20]
Adverse effects
[edit]Melatonin appears to cause very few side effects as tested in the short term, up to three months, at low doses.[clarification needed][dubious – discuss] Two systematic reviews found no adverse effects of exogenous melatonin in several clinical trials, and comparative trials found the adverse effects headaches, dizziness, nausea, and drowsiness were reported about equally for both melatonin and placebo.[43][44] Prolonged-release melatonin is safe with long-term use of up to 12 months.[11] Although not recommended for long-term use beyond this,[45] low-dose melatonin is generally safer, and a better alternative, than many prescription and over-the-counter sleep aids if a sleeping medication must be used for an extended period of time.[citation needed] Low doses of melatonin are usually sufficient to produce a hypnotic effect in most people. Higher doses do not appear to result in a stronger effect but instead appear to cause drowsiness for a longer period of time.[46]
There is emerging evidence that the timing of taking exogenous melatonin in relation to food is also an important factor.[47] Specifically, taking exogenous melatonin shortly after a meal is correlated with impaired glucose tolerance. Therefore, Rubio-Sastre and colleagues recommend waiting at least 2 hours after the last meal before taking a melatonin supplement.[48]
Melatonin can cause nausea, next-day grogginess, and irritability.[49] In autoimmune disorders, evidence is conflicting whether melatonin supplementation may ameliorate or exacerbate symptoms due to immunomodulation.[50][51][needs update]
Melatonin can lower follicle-stimulating hormone levels.[52] Melatonin's effects on human reproduction remain unclear.[53]
Some supplemental melatonin users report an increase in vivid dreaming. Extremely high doses of melatonin increased REM sleep time and dream activity in people both with and without narcolepsy.[54]
Increased use of melatonin in the 21st century has significantly increased reports of melatonin overdose, calls to poison control centers, and related emergency department visits for children. The number of children who unintentionally ingested melatonin supplements in the US has increased 530% from 2012 to 2021. Over 4,000 reported ingestions required a hospital stay, and 287 children required intensive care. The American Academy of Sleep Medicine says there is little evidence that melatonin supplementation is effective in treating insomnia in healthy children.[42]
Overdose
[edit]Melatonin appears to be relatively safe in overdose.[8] It has been administered at daily doses of up to 300 mg without causing clinically significant adverse reactions in the literature.[8] The most commonly reported adverse effect of melatonin overdose is somnolence.[8] Upon melatonin overdose, drowsiness may be expected and the compound should be cleared within 12 hours.[8] No special treatment is needed for melatonin overdose.[8]
Interactions
[edit]Melatonin is metabolized mainly by CYP1A enzymes. As such, inhibitors and inducers of CYP1A enzymes, such as CYP1A2, can modify melatonin metabolism and exposure.[8] As an example, the CYP1A2 and CYP2C19 inhibitor fluvoxamine increases melatonin peak levels by 12-fold and overall exposure by 17-fold and this combination should be avoided.[8] CYP1A2 inducers like cigarette smoking, carbamazepine, and rifampicin may reduce melatonin exposure due to induction of CYP1A2.[8]
In those taking warfarin, some evidence suggests there may exist a potentiating interaction, increasing the anticoagulant effect of warfarin and the risk of bleeding.[55]
Pharmacology
[edit]Pharmacodynamics
[edit]Melatonin acts as an agonist of the melatonin MT1 and MT2 receptors, the biological targets of endogenous melatonin.[21] Endogenous melatonin is normally secreted from the pineal gland of the brain.[21] Melatonin is thought to activate melatonin receptors in the suprachiasmatic nucleus of the hypothalamus to regulate the circadian clock and sleep–wake cycles.[21] When used several hours before sleep according to the phase response curve for melatonin in humans, small amounts (0.3 mg[56]) of melatonin shift the circadian clock earlier, thus promoting earlier sleep onset and morning awakening.[57]
Pharmacokinetics
[edit]Absorption
[edit]The bioavailability of melatonin is between 2.5 and 50%.[6][7] Melatonin is rapidly absorbed and distributed, reaching peak plasma concentrations after 60 minutes of administration, and is then eliminated.[6] Usual doses of exogenous melatonin of 1 to 12 mg produce melatonin concentrations 10 to 100 times higher than endogenous peak levels.[7]
Distribution
[edit]The plasma protein binding of melatonin is approximately 60%.[8][7] It is mainly bound to albumin, α1-acid glycoprotein, and high-density lipoprotein.[8]
The membrane transport proteins that move melatonin across a membrane include, but are not limited to, glucose transporters, including GLUT1, and the proton-driven oligopeptide transporters PEPT1 and PEPT2.[58][59]
Metabolism
[edit]Melatonin is metabolized in the liver by cytochrome P450 enzyme CYP1A2 to 6-hydroxymelatonin. Metabolites are conjugated with sulfuric acid or glucuronic acid for excretion in the urine. Some of the metabolites formed via the reaction of melatonin with a free radical include cyclic 3-hydroxymelatonin, N1-acetyl-N2-formyl-5-methoxykynuramine (AFMK), and N1-acetyl-5-methoxykynuramine (AMK).[58][59]
Elimination
[edit]In humans, 90% of orally administered exogenous melatonin is cleared in a single passage through the liver, a small amount is excreted in urine, and a small amount is found in saliva.[13] Melatonin is excreted in the urine 2 to 5% as the unchanged drug.[6][8]
Melatonin has an elimination half-life of about 20 to 60 minutes.[22][7][9][10] The half-life of prolonged-release melatonin (Circadin) is 3.5 to 4 hours.[11][8]
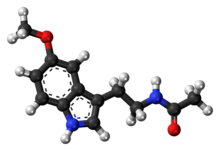
Chemistry
[edit]Melatonin, also known as N-acetyl-5-methoxytryptamine, is a substituted tryptamine and a derivative of serotonin (5-hydroxytryptamine). It is structurally related to N-acetylserotonin (normelatonin; N-acetyl-5-hydroxytryptamine), which is the chemical intermediate between serotonin and melatonin in the body. Synthetic melatonin receptor agonists used in medicine like ramelteon, tasimelteon, agomelatine, and piromelatine (still in clinical trials) are analogues of melatonin.
History
[edit]The first patent for its use in circadian rhythm disorders was granted in 1987 to Roger V Short and Stuart Armstrong at Monash University,[60] and the first patent for its use as a low-dose sleep aid was granted to Richard Wurtman at MIT in 1995.[61] Around the same time, the hormone got a lot of press as a possible treatment for many illnesses.[62] The New England Journal of Medicine editorialized in 2000: "With these recent careful and precise observations in blind persons, the true potential of melatonin is becoming evident, and the importance of the timing of treatment is becoming clear."[63]
It was approved for medical use in the European Union in 2007.[8]
Society and culture
[edit]Melatonin is categorized by the US Food and Drug Administration (FDA) as a dietary supplement, and is sold over-the-counter in both the US and Canada.[13] FDA regulations applying to medications are not applicable to melatonin,[64] though the FDA has found false claims that it cures cancer.[65] As melatonin may cause harm in combination with certain medications or in the case of certain disorders, a doctor or pharmacist should be consulted before making a decision to take melatonin.[30] In many countries, melatonin is recognized as a neurohormone and it cannot be sold over-the-counter.[66] According to Harriet Hall caution is advisable, since quality control is a documented problem. 71% of products did not contain within 10% of the labelled amount of melatonin, with variations ranging from -83% to +478%, lot-to-lot variability was as high as 465%, and the discrepancies were not correlated to any manufacturer or product type. To make matters worse, 8 out of 31 products were contaminated with the neurotransmitter serotonin.[67][68]
Formerly, melatonin was derived from animal pineal tissue, such as bovine. It is now synthetic, which limits the risk of contamination or the means of transmitting infectious material.[64][69]
Melatonin is the most popular over-the-counter sleep remedy in the United States, resulting in sales in excess of US$400 million during 2017.[70] In 2021, it was the 257th most commonly prescribed medication in the US, with more than 1 million prescriptions.[26][27]
Beverages and snacks containing melatonin were being sold in grocery stores, convenience stores, and clubs in May 2011.[71] The FDA considered whether these food products could continue to be sold with the label "dietary supplements". On 13 January 2010, it issued a Warning Letter to Innovative Beverage, creators of several beverages marketed as drinks, stating that melatonin, while legal as a dietary supplement, was not approved as a food additive.[72] Bebida Beverage Company received a warning letter in 2015 for selling a melatonin-containing beverage.[73]
Research
[edit]Some research supports an antidepressant and anxiolytic effect of melatonin.[74][75] It has also been used to aid in the treatment of manic episodes in bipolar disorder, although evidence for its effectiveness is still inconsistent.[76]
Other studies have shown that melatonin may help reduce some types of headaches, epigastric pain and heartburn.[77][78][79] There have also been studies trying to prove the effectiveness of melatonin in relation to epilepsy, dysmenorrhea, delirium, and tinnitus, but little to no beneficial role has been found.[80][81][82][83] Melatonin has also been tested as a treatment for cancer, but the National Cancer Institute found insufficient evidence for it. However, further research found it to slightly improve survival of patients and to alleviate chemotherapy-related side effects.[84][85][86][87]
Both animal[88] and human[89][90][91] studies have shown melatonin to protect against radiation-induced cellular damage. Melatonin and its metabolites protect organisms from oxidative stress by scavenging reactive oxygen species which are generated during exposure.[92] Nearly 70% of biological damage caused by ionizing radiation is estimated to be attributable to the creation of free radicals, especially the hydroxyl radical that attacks DNA, proteins, and cellular membranes. Melatonin has been described as a broadly protective, readily available, and orally self-administered antioxidant that is without known major side effects.[93]
References
[edit]- ^ "Melatonin – Drugs.com". Drugs.com. Retrieved 12 October 2018.
- ^ "Melatonin". Sleepdex. Retrieved 17 August 2011.
- ^ a b https://www.tga.gov.au/resources/auspar/auspar-melatonin-1 [bare URL]
- ^ a b c "Pros and cons of melatonin". Mayo Clinic. Retrieved 20 August 2022.
- ^ https://www.tga.gov.au/resources/auspar/auspar-melatonin-link-immela-melakso-voquily [bare URL]
- ^ a b c d Tordjman S, Chokron S, Delorme R, Charrier A, Bellissant E, Jaafari N, et al. (April 2017). "Melatonin: Pharmacology, Functions and Therapeutic Benefits". Current Neuropharmacology. 15 (3): 434–443. doi:10.2174/1570159X14666161228122115. PMC 5405617. PMID 28503116.
- ^ a b c d e f Lalanne S, Fougerou-Leurent C, Anderson GM, Schroder CM, Nir T, Chokron S, et al. (February 2021). "Melatonin: From Pharmacokinetics to Clinical Use in Autism Spectrum Disorder". Int J Mol Sci. 22 (3): 1490. doi:10.3390/ijms22031490. PMC 7867370. PMID 33540815.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y Circadin: EPAR - Product Information ANNEX I - SUMMARY OF PRODUCT CHARACTERISTICS (Report). European Medicines Agency (EMA). 2 February 2021. EMEA/H/C/000695 - IA/0066. As PDF. Archived 31 October 2022 at the Wayback Machine Text was copied from this source which is copyright European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
- ^ a b c d e f g h Auld F, Maschauer EL, Morrison I, Skene DJ, Riha RL (August 2017). "Evidence for the efficacy of melatonin in the treatment of primary adult sleep disorders" (PDF). Sleep Medicine Reviews. 34: 10–22. doi:10.1016/j.smrv.2016.06.005. hdl:20.500.11820/0e890bda-4b1d-4786-a907-a03b1580fd07. PMID 28648359.
- ^ a b c Hardeland R, Poeggeler B, Srinivasan V, Trakht I, Pandi-Perumal SR, Cardinali DP (2008). "Melatonergic drugs in clinical practice". Arzneimittelforschung. 58 (1): 1–10. doi:10.1055/s-0031-1296459. PMID 18368944. S2CID 38857779.
- ^ a b c d e f Lyseng-Williamson KA (November 2012). "Melatonin prolonged release: in the treatment of insomnia in patients aged ≥55 years". Drugs & Aging. 29 (11): 911–23. doi:10.1007/s40266-012-0018-z. PMID 23044640. S2CID 1403262.
- ^ a b Faraone SV (2014). ADHD: Non-Pharmacologic Interventions, An Issue of Child and Adolescent Psychiatric Clinics of North America, E-Book. Elsevier Health Sciences. p. 888. ISBN 978-0-323-32602-5.
- ^ a b c Buscemi N, Vandermeer B, Pandya R, Hooton N, Tjosvold L, Hartling L, et al. (November 2004). "Melatonin for treatment of sleep disorders" (PDF). Evidence Report/Technology Assessment No. 108. (Prepared by the University of Alberta Evidence-based Practice Center, Under Contract No. 290-02-0023.) AHRQ Publication No. 05-E002-2. Rockville, MD: Agency for Healthcare Research and Quality (108). Agency for Healthcare Research and Quality (AHRQ), US Department of Health and Human Services: 1–7. doi:10.1037/e439412005-001. PMC 4781368. PMID 15635761. Retrieved 5 June 2013.
- ^ a b Matheson E, Hainer BL (July 2017). "Insomnia: Pharmacologic Therapy". American Family Physician. 96 (1): 29–35. PMID 28671376.
- ^ a b c d British national formulary: BNF 76 (76 ed.). Pharmaceutical Press. 2018. pp. 482–483. ISBN 978-0-85711-338-2.
- ^ Brasure M, MacDonald R, Fuchs E, Olson CM, Carlyle M, Diem S, et al. (2015). "Management of Insomnia Disorder[Internet]". AHRQ Comparative Effectiveness Reviews. 15 (16): EHC027–EF. PMID 26844312.
Evidence for benzodiazepine hypnotics, melatonin agonists in the general adult population, and most pharmacologic interventions in older adults was generally insufficient
- ^ a b c d e "Melatonin: Side Effects, Uses, Dosage (Kids/Adults)". Drugs.com. Retrieved 9 January 2019.
- ^ a b "Slenyto EPAR". European Medicines Agency (EMA). 17 September 2018. Retrieved 31 May 2020. Text was copied from this source which is copyright European Medicines Agency. Reproduction is authorized, provided the source is acknowledged.
- ^ a b "Summary Safety Review – MELATONIN (N-acetyl-5-methoxytryptamine) – Review of the Safety of Melatonin in Children and Adolescents". Government of Canada. Health Canada. 10 December 2015. Retrieved 9 January 2019.
- ^ a b c "Melatonin- Oral". Government of Canada. Health Canada. 28 August 2018. Archived from the original on 1 April 2019. Retrieved 9 January 2019.
- ^ a b c d e Pevet P, Challet E, Felder-Schmittbuhl MP (2021). "Melatonin and the circadian system: Keys for health with a focus on sleep". The Human Hypothalamus: Anterior Region. Handbook of Clinical Neurology. Vol. 179. pp. 331–343. doi:10.1016/B978-0-12-819975-6.00021-2. ISBN 9780128199756. PMID 34225973. S2CID 235744969.
- ^ a b "Melatonin". www.drugbank.ca. Retrieved 29 January 2019.
- ^ "Australian Public Assessment Report for Melatonin" (PDF). Australian Government Department of Health and Ageing Therapeutic Goods Administration. January 2011. pp. 2, 4. Retrieved 9 January 2019.
Monotherapy for the short term treatment of primary insomnia characterised by poor quality of sleep in patients who are aged 55 or over.
- ^ Williams WP, McLin DE, Dressman MA, Neubauer DN (September 2016). "Comparative Review of Approved Melatonin Agonists for the Treatment of Circadian Rhythm Sleep-Wake Disorders". Pharmacotherapy. 36 (9): 1028–41. doi:10.1002/phar.1822. PMC 5108473. PMID 27500861.
- ^ Atkin T, Comai S, Gobbi G (April 2018). "Drugs for Insomnia beyond Benzodiazepines: Pharmacology, Clinical Applications, and Discovery". Pharmacol Rev. 70 (2): 197–245. doi:10.1124/pr.117.014381. PMID 29487083. S2CID 3578916.
- ^ a b "The Top 300 of 2021". ClinCalc. Archived from the original on 15 January 2024. Retrieved 14 January 2024.
- ^ a b "Melatonin - Drug Usage Statistics". ClinCalc. Retrieved 14 January 2024.
- ^ Carney CE, Lau PH, Kutana S (2023). "Chapter 10: Insomnia". In Hupp S, Santa Maria CL (eds.). Pseudoscience in Therapy: A Skeptical Field Guide. Cambridge University Press. pp. 147–148. doi:10.1017/9781009000611.011. ISBN 9781009000611.
- ^ a b Wade A, Downie S (October 2008). "Prolonged-release melatonin for the treatment of insomnia in patients over 55 years". Expert Opin Investig Drugs. 17 (10): 1567–72. doi:10.1517/13543784.17.10.1567. PMID 18808316. S2CID 71158456.
- ^ a b Herxheimer A, Petrie KJ (2002). "Melatonin for the prevention and treatment of jet lag". The Cochrane Database of Systematic Reviews. 2010 (2): CD001520. doi:10.1002/14651858.CD001520. PMC 8958662. PMID 12076414.
- ^ a b Liira J, Verbeek JH, Costa G, Driscoll TR, Sallinen M, Isotalo LK, et al. (August 2014). "Pharmacological interventions for sleepiness and sleep disturbances caused by shift work". The Cochrane Database of Systematic Reviews. 2014 (8): CD009776. doi:10.1002/14651858.CD009776.pub2. PMC 10025070. PMID 25113164.
- ^ McCarter SJ, Boswell CL, St Louis EK, Dueffert LG, Slocumb N, Boeve BF, et al. (March 2013). "Treatment outcomes in REM sleep behavior disorder". Sleep Medicine (Review). 14 (3): 237–42. doi:10.1016/j.sleep.2012.09.018. PMC 3617579. PMID 23352028.
- ^ McKeith IG, Boeve BF, Dickson DW, Halliday G, Taylor JP, Weintraub D, et al. (July 2017). "Diagnosis and management of dementia with Lewy bodies: Fourth consensus report of the DLB Consortium". Neurology (Review). 89 (1): 88–100. doi:10.1212/WNL.0000000000004058. PMC 5496518. PMID 28592453.
- ^ Boot BP (2015). "Comprehensive treatment of dementia with Lewy bodies". Alzheimer's Research & Therapy (Review). 7 (1): 45. doi:10.1186/s13195-015-0128-z. PMC 4448151. PMID 26029267.
- ^ a b Gilat M, Marshall NS, Testelmans D, Buyse B, Lewis SJ (January 2022). "A critical review of the pharmacological treatment of REM sleep behavior disorder in adults: time for more and larger randomized placebo-controlled trials". J Neurol. 269 (1): 125–148. doi:10.1007/s00415-020-10353-0. PMC 8739295. PMID 33410930.
- ^ McCleery J, Sharpley AL (November 2020). "Pharmacotherapies for sleep disturbances in dementia". The Cochrane Database of Systematic Reviews. 2020 (11): CD009178. doi:10.1002/14651858.CD009178.pub4. PMC 8094738. PMID 33189083.
- ^ Spinedi E, Cardinali DP (2019). "Neuroendocrine-Metabolic Dysfunction and Sleep Disturbances in Neurodegenerative Disorders: Focus on Alzheimer's Disease and Melatonin". Neuroendocrinology. 108 (4): 354–364. doi:10.1159/000494889. hdl:11336/86560. PMID 30368508. S2CID 53101746.
- ^ Gao C, Scullin MK, Bliwise DL (2019). "Mild Cognitive Impairment and Dementia". In Savard J, Ouellet MC (eds.). Handbook of Sleep Disorders in Medical Conditions. Academic Press. pp. 253–276. doi:10.1016/b978-0-12-813014-8.00011-1. ISBN 978-0-12-813014-8. S2CID 88265944.
- ^ Soca R (28 February 2021). "Melatonin Product Availability". Keldik Sleep Circadian and Performance. Archived from the original on 27 May 2022. Retrieved 11 April 2022.
- ^ a b Kolli AR, Kuczaj AK, Calvino-Martin F, Hoeng J (May 2024). "Simulated pharmacokinetics of inhaled caffeine and melatonin from existing products indicate the lack of dosimetric considerations". Food and Chemical Toxicology. 187: 114601. doi:10.1016/j.fct.2024.114601. PMID 38493979.
- ^ Posadzki PP, Bajpai R, Kyaw BM, Roberts NJ, Brzezinski A, Christopoulos GI, et al. (February 2018). "Melatonin and health: an umbrella review of health outcomes and biological mechanisms of action". BMC Medicine. 16 (1): 18. doi:10.1186/s12916-017-1000-8. PMC 5798185. PMID 29397794.
- ^ a b Brooks M (23 September 2022). "Experts Issue Health Warning About Giving Melatonin to Kids". Medscape.
- ^ Buscemi N, Vandermeer B, Hooton N, Pandya R, Tjosvold L, Hartling L, et al. (December 2005). "The efficacy and safety of exogenous melatonin for primary sleep disorders. A meta-analysis". Journal of General Internal Medicine. 20 (12): 1151–8. doi:10.1111/j.1525-1497.2005.0243.x. PMC 1490287. PMID 16423108.
- ^ Buscemi N, Vandermeer B, Hooton N, Pandya R, Tjosvold L, Hartling L, et al. (February 2006). "Efficacy and safety of exogenous melatonin for secondary sleep disorders and sleep disorders accompanying sleep restriction: meta-analysis". BMJ. 332 (7538): 385–93. doi:10.1136/bmj.38731.532766.F6. PMC 1370968. PMID 16473858.
- ^ "Melatonin: What You Need To Know". NCCIH. National Institutes of Health. Retrieved 2 July 2021.
- ^ Database of Abstracts of Reviews of Effects (DARE): Quality-assessed Reviews [Internet]. York (UK): Centre for Reviews and Dissemination (UK); 1995. Optimal dosages for melatonin supplementation therapy in older adults: a systematic review of current literature. 2014.
- ^ Garaulet M, Qian J, Florez JC, Arendt J, Saxena R, Scheer FA (March 2020). "Melatonin Effects on Glucose Metabolism: Time To Unlock the Controversy". Trends in Endocrinology and Metabolism. 31 (3): 192–204. doi:10.1016/j.tem.2019.11.011. PMC 7349733. PMID 31901302.
- ^ Rubio-Sastre P, Scheer FA, Gómez-Abellán P, Madrid JA, Garaulet M (October 2014). "Acute melatonin administration in humans impairs glucose tolerance in both the morning and evening". Sleep. 37 (10): 1715–9. doi:10.5665/sleep.4088. PMC 4173928. PMID 25197811.
- ^ Bauer B. "Melatonin side effects: What are the risks?". Mayo Clinic. Retrieved 17 August 2011.
- ^ Morera AL, Henry M, de La Varga M (2001). "[Safety in melatonin use]" [Safety in melatonin use]. Actas Españolas de Psiquiatría (in Spanish). 29 (5): 334–7. PMID 11602091.
- ^ Terry PD, Villinger F, Bubenik GA, Sitaraman SV (January 2009). "Melatonin and ulcerative colitis: evidence, biological mechanisms, and future research". Inflammatory Bowel Diseases. 15 (1): 134–40. doi:10.1002/ibd.20527. PMID 18626968.
- ^ Juszczak M, Michalska M (2006). "[The effect of melatonin on prolactin, luteinizing hormone (LH), and follicle-stimulating hormone (FSH) synthesis and secretion]" [The effect of melatonin on prolactin, luteinizing hormone (LH), and follicle-stimulating hormone (FSH) synthesis and secretion]. Postepy Higieny I Medycyny Doswiadczalnej (in Polish). 60: 431–8. PMID 16921343. Archived from the original on 2 November 2014. Retrieved 24 December 2013.
- ^ Srinivasan V, Spence WD, Pandi-Perumal SR, Zakharia R, Bhatnagar KP, Brzezinski A (December 2009). "Melatonin and human reproduction: shedding light on the darkness hormone". Gynecological Endocrinology. 25 (12): 779–85. doi:10.3109/09513590903159649. PMID 19905996. S2CID 3442003.
- ^ Lewis A (1999). Melatonin and the Biological Clock. McGraw-Hill. p. 23. ISBN 978-0-87983-734-1.
- ^ "Melatonin – Special Subjects". Merck Manuals Professional Edition.
- ^ Mundey K, Benloucif S, Harsanyi K, Dubocovich ML, Zee PC (October 2005). "Phase-dependent treatment of delayed sleep phase syndrome with melatonin". Sleep. 28 (10): 1271–8. doi:10.1093/sleep/28.10.1271. PMID 16295212.
- ^ Terman MR, Wirz-Justice A (2009). Chronotherapeutics for Affective Disorders: A Clinician's Manual for Light and Wake Therapy. Basel: S Karger Pub. p. 71. ISBN 978-3-8055-9120-1.
- ^ a b Jockers R, Delagrange P, Dubocovich ML, Markus RP, Renault N, Tosini G, et al. (September 2016). "Update on melatonin receptors: IUPHAR Review 20". British Journal of Pharmacology. 173 (18): 2702–25. doi:10.1111/bph.13536. PMC 4995287. PMID 27314810.
- ^ a b Mayo JC, Sainz RM, González-Menéndez P, Hevia D, Cernuda-Cernuda R (November 2017). "Melatonin transport into mitochondria". Cellular and Molecular Life Sciences. 74 (21): 3927–3940. doi:10.1007/s00018-017-2616-8. PMC 11107582. PMID 28828619. S2CID 10920415.
- ^ "Method for minimizing disturbances in circadian rhythms of bodily performance and function - Patent US-4665086-A - PubChem". pubchem.ncbi.nlm.nih.gov. Retrieved 16 April 2022.
- ^ US patent 5449683, Wurtman RJ, "Methods of inducing sleep using melatonin", issued 12 September 1995, assigned to Massachusetts Institute of Technology
- ^ Arendt J (August 2005). "Melatonin: characteristics, concerns, and prospects". Journal of Biological Rhythms. 20 (4): 291–303. doi:10.1177/0748730405277492. PMID 16077149. S2CID 19011222.
There is very little evidence in the short term for toxicity or undesirable effects in humans. The extensive promotion of the miraculous powers of melatonin in the recent past did a disservice to acceptance of its genuine benefits.
- ^ Arendt J (October 2000). "Melatonin, circadian rhythms, and sleep". The New England Journal of Medicine. 343 (15): 1114–6. doi:10.1056/NEJM200010123431510. PMID 11027748.
- ^ a b Altun A, Ugur-Altun B (May 2007). "Melatonin: therapeutic and clinical utilization". International Journal of Clinical Practice. 61 (5): 835–45. doi:10.1111/j.1742-1241.2006.01191.x. PMID 17298593. S2CID 18050554.
- ^ "187 Fake Cancer 'Cures' Consumers Should Avoid". U.S. Food and Drug Administration. Archived from the original on 2 May 2017. Retrieved 20 May 2020.
- ^ Guardiola-Lemaître B (December 1997). "Toxicology of melatonin". Journal of Biological Rhythms. 12 (6): 697–706. doi:10.1177/074873049701200627. PMID 9406047. S2CID 31090576.
- ^ Hall H (15 December 2020). "Melatonin Melatonin supplements are increasingly popular, but the evidence is weak and mixed". Science-Based Medicine. Science Based Medicine. Retrieved 24 December 2020.
- ^ Erland LA, Saxena PK (February 2017). "Melatonin Natural Health Products and Supplements: Presence of Serotonin and Significant Variability of Melatonin Content". Journal of Clinical Sleep Medicine. 13 (2): 275–281. doi:10.5664/jcsm.6462. PMC 5263083. PMID 27855744.
- ^ "Melatonin". Drugs.com. Retrieved 17 August 2011.
- ^ Loria K. "Does Melatonin Really Help You Sleep?". Consumer Reports. Retrieved 16 March 2019.
- ^ Louis CS (14 May 2011). "Dessert, Laid-Back and Legal". The New York Times.
- ^ Rodriguez RR (13 January 2010). "Warning Letter". Inspections, Compliance, Enforcement, and Criminal Investigations. U.S. Food and Drug Administration. Archived from the original on 12 January 2017.
- ^ "Bebida Beverage Company". U.S. Food and Drug Administration. 4 March 2015. Archived from the original on 1 June 2020. Retrieved 8 December 2017.
- ^ Valdés-Tovar M, Estrada-Reyes R, Solís-Chagoyán H, Argueta J, Dorantes-Barrón AM, Quero-Chávez D, et al. (August 2018). "Circadian modulation of neuroplasticity by melatonin: a target in the treatment of depression". British Journal of Pharmacology. 175 (16): 3200–3208. doi:10.1111/bph.14197. PMC 6057892. PMID 29512136.
- ^ Hansen MV, Halladin NL, Rosenberg J, Gögenur I, Møller AM (8 December 2020). "Melatonin for pre- and postoperative anxiety in adults". The Cochrane Database of Systematic Reviews. 2020 (12): CD009861. doi:10.1002/14651858.CD009861.pub3. PMC 8092422. PMID 33319916.
- ^ Bartoli F, Cavaleri D, Bachi B, Moretti F, Riboldi I, Crocamo C, et al. (September 2021). "Repurposed drugs as adjunctive treatments for mania and bipolar depression: A meta-review and critical appraisal of meta-analyses of randomized placebo-controlled trials". Journal of Psychiatric Research. 143: 230–238. doi:10.1016/j.jpsychires.2021.09.018. PMID 34509090. S2CID 237485915.
- ^ Peres MF, Masruha MR, Zukerman E, Moreira-Filho CA, Cavalheiro EA (April 2006). "Potential therapeutic use of melatonin in migraine and other headache disorders". Expert Opinion on Investigational Drugs. 15 (4): 367–75. doi:10.1517/13543784.15.4.367. PMID 16548786. S2CID 28114683.
- ^ Evers S, Goadsby PJ (2005). "Review: Hypnic headache" (PDF). Practical Neurology. 5 (3): 144–49. doi:10.1111/j.1474-7766.2005.00301.x. S2CID 1196313. Retrieved 12 January 2018.
- ^ Kandil TS, Mousa AA, El-Gendy AA, Abbas AM (January 2010). "The potential therapeutic effect of melatonin in Gastro-Esophageal Reflux Disease". BMC Gastroenterology. 10: 7. doi:10.1186/1471-230X-10-7. PMC 2821302. PMID 20082715.
- ^ Brigo F, Igwe SC, Del Felice A (August 2016). "Melatonin as add-on treatment for epilepsy". The Cochrane Database of Systematic Reviews. 2016 (8): CD006967. doi:10.1002/14651858.CD006967.pub4. PMC 7386917. PMID 27513702.
- ^ Pattanittum P, Kunyanone N, Brown J, Sangkomkamhang US, Barnes J, Seyfoddin V, et al. (March 2016). "Dietary supplements for dysmenorrhoea". The Cochrane Database of Systematic Reviews. 2016 (3): CD002124. doi:10.1002/14651858.CD002124.pub2. PMC 7387104. PMID 27000311.
- ^ Siddiqi N, Harrison JK, Clegg A, Teale EA, Young J, Taylor J, et al. (March 2016). "Interventions for preventing delirium in hospitalised non-ICU patients" (PDF). The Cochrane Database of Systematic Reviews. 2016 (3): CD005563. doi:10.1002/14651858.CD005563.pub3. PMC 10431752. PMID 26967259.
- ^ Miroddi M, Bruno R, Galletti F, Calapai F, Navarra M, Gangemi S, et al. (March 2015). "Clinical pharmacology of melatonin in the treatment of tinnitus: a review". European Journal of Clinical Pharmacology. 71 (3): 263–70. doi:10.1007/s00228-015-1805-3. PMID 25597877. S2CID 16466238.
- ^ PDQ Integrative, Alternative, and Complementary Therapies Editorial Board (May 2013). "Topics in complementary and alternative therapies". PDQ Cancer Information Summaries [Internet]. National Cancer Institute, National Institutes of Health. PMID 26389506.
- ^ Lim S, Park S, Koyanagi A, Yang JW, Jacob L, Yon DK, et al. (February 2022). "Effects of exogenous melatonin supplementation on health outcomes: An umbrella review of meta-analyses based on randomized controlled trials" (PDF). Pharmacological Research. 176: 106052. doi:10.1016/j.phrs.2021.106052. PMID 34999224. S2CID 263492993. Archived from the original (PDF) on 31 March 2023. Retrieved 24 January 2023.
- ^ Posadzki PP, Bajpai R, Kyaw BM, Roberts NJ, Brzezinski A, Christopoulos GI, et al. (February 2018). "Melatonin and health: an umbrella review of health outcomes and biological mechanisms of action". BMC Medicine. 16 (1): 18. doi:10.1186/s12916-017-1000-8. PMC 5798185. PMID 29397794.
- ^ Wang YM, Jin BZ, Ai F, Duan CH, Lu YZ, Dong TF, et al. (May 2012). "The efficacy and safety of melatonin in concurrent chemotherapy or radiotherapy for solid tumors: a meta-analysis of randomized controlled trials". Cancer Chemotherapy and Pharmacology. 69 (5): 1213–1220. doi:10.1007/s00280-012-1828-8. PMID 22271210. S2CID 38488628.
- ^ Meltz ML, Reiter RJ, Herman TS, Kumar KS (March 1999). "Melatonin and protection from whole-body irradiation: survival studies in mice". Mutation Research. 425 (1): 21–7. Bibcode:1999MRFMM.425...21V. doi:10.1016/S0027-5107(98)00246-2. PMID 10082913.
- ^ Reiter RJ, Herman TS, Meltz ML (December 1996). "Melatonin and radioprotection from genetic damage: in vivo/in vitro studies with human volunteers". Mutation Research. 371 (3–4): 221–8. doi:10.1016/S0165-1218(96)90110-X. PMID 9008723.
- ^ Pattanittum P, Kunyanone N, Brown J, Sangkomkamhang US, Barnes J, Seyfoddin V, et al. (March 2016). "Dietary supplements for dysmenorrhoea". The Cochrane Database of Systematic Reviews. 2016 (3): CD002124. doi:10.1002/14651858.cd002124.pub2. PMC 7387104. PMID 27000311.
- ^ Reiter RJ, Herman TS, Meltz ML (February 1998). "Melatonin reduces gamma radiation-induced primary DNA damage in human blood lymphocytes". Mutation Research. 397 (2): 203–8. Bibcode:1998MRFMM.397..203V. doi:10.1016/S0027-5107(97)00211-X. PMID 9541644.
- ^ Tan DX, Manchester LC, Terron MP, Flores LJ, Reiter RJ (January 2007). "One molecule, many derivatives: a never-ending interaction of melatonin with reactive oxygen and nitrogen species?". Journal of Pineal Research. 42 (1): 28–42. doi:10.1111/j.1600-079X.2006.00407.x. PMID 17198536. S2CID 40005308.
- ^ Shirazi A, Ghobadi G, Ghazi-Khansari M (July 2007). "A radiobiological review on melatonin: a novel radioprotector". Journal of Radiation Research. 48 (4): 263–72. Bibcode:2007JRadR..48..263S. doi:10.1269/jrr.06070. PMID 17641465.