Passive immunity
In immunology, passive immunity is the transfer of active humoral immunity of ready-made antibodies. Passive immunity can occur naturally, when maternal antibodies are transferred to the fetus through the placenta, and it can also be induced artificially, when high levels of antibodies specific to a pathogen or toxin (obtained from humans, horses, or other animals) are transferred to non-immune persons through blood products that contain antibodies, such as in immunoglobulin therapy or antiserum therapy.[1] Passive immunization is used when there is a high risk of infection and insufficient time for the body to develop its own immune response, or to reduce the symptoms of ongoing or immunosuppressive diseases.[2] Passive immunization can be provided when people cannot synthesize antibodies, and when they have been exposed to a disease that they do not have immunity against.[3]
Naturally acquired
[edit]Maternal passive immunity
[edit]Maternal passive immunity is a type of naturally acquired passive immunity, and refers to antibody-mediated immunity conveyed to a fetus or infant by its mother. Naturally acquired passive immunity can be provided during pregnancy, and through breastfeeding.[4] In humans, maternal antibodies (MatAb) are passed through the placenta to the fetus by an FcRn receptor on placental cells. This occurs predominately during the third trimester of pregnancy, and thus is often reduced in babies born prematurely. Immunoglobulin G (IgG) is the only antibody isotype that can pass through the human placenta, and is the most common antibody of the five types of antibodies found in the body. IgG antibodies protects against bacterial and viral infections in fetuses. Immunization is often required shortly following birth to prevent diseases in newborns such as tuberculosis, hepatitis B, polio, and pertussis, however, maternal IgG can inhibit the induction of protective vaccine responses throughout the first year of life. This effect is usually overcome by secondary responses to booster immunization.[5] Maternal antibodies protect against some diseases, such as measles, rubella, and tetanus, more effectively than against others, such as polio and pertussis.[6] Maternal passive immunity offers immediate protection, though protection mediated by maternal IgG typically only lasts up to a year.[6]
Passive immunity is also provided through colostrum and breast milk, which contain IgA antibodies that are transferred to the gut of the infant, providing local protection against disease causing bacteria and viruses until the newborn can synthesize its own antibodies.[7] Protection mediated by IgA is dependent on the length of time that an infant is breastfed, which is one of the reasons the World Health Organization recommends breastfeeding for at least the first two years of life.[8]
Other species besides humans transfer maternal antibodies before birth, including primates and lagomorphs (which includes rabbits and hares).[9] In some of these species IgM can be transferred across the placenta as well as IgG. All other mammalian species predominantly or solely transfer maternal antibodies after birth through milk. In these species, the neonatal gut is able to absorb IgG for hours to days after birth. However, after a period of time the neonate can no longer absorb maternal IgG through their gut, an event that is referred to as "gut closure". If a neonatal animal does not receive adequate amounts of colostrum prior to gut closure, it does not have a sufficient amount of maternal IgG in its blood to fight off common diseases. This condition is referred to as failure of passive transfer. It can be diagnosed by measuring the amount of IgG in a newborn's blood, and is treated with intravenous administration of immunoglobulins. If not treated, it can be fatal.[citation needed]
Other
[edit]A preprint suggested that (SARS-CoV-2) antibodies in or transmitted through the air are an unrecognized mechanism by which, transferred, passive immune protection occurs.[10][better source needed]
Antibodies from vaccination can be present in saliva and thereby may have utility in preventing infection.[11][better source needed]
Artificially acquired
[edit]Artificially acquired passive immunity is a short-term immunization achieved by the transfer of antibodies, which can be administered in several forms; as human or animal blood plasma or serum, as pooled human immunoglobulin for intravenous (IVIG) or intramuscular (IG) use, as high-titer human IVIG or IG from immunized donors or from donors recovering from the disease, and as monoclonal antibodies (MAb). Passive transfer is used to prevent disease or used prophylactically in the case of immunodeficiency diseases, such as hypogammaglobulinemia.[12][13] It is also used in the treatment of several types of acute infection, and to treat poisoning.[2] Immunity derived from passive immunization lasts for a few weeks to three to four months.[14][15] There is also a potential risk for hypersensitivity reactions, and serum sickness, especially from gamma globulin of non-human origin.[7] Passive immunity provides immediate protection, but the body does not develop memory; therefore, the patient is at risk of being infected by the same pathogen later unless they acquire active immunity or vaccination.[7]
History and applications of artificial passive immunity
[edit]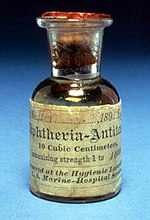
In 1888 Emile Roux and Alexandre Yersin showed that the clinical effects of diphtheria were caused by diphtheria toxin and, following the 1890 discovery of an antitoxin-based immunity to diphtheria and tetanus by Emil Adolf von Behring and Kitasato Shibasaburō, antitoxin became the first major success of modern therapeutic immunology.[16][17] Shibasaburo and von Behring immunized guinea pigs with the blood products from animals that had recovered from diphtheria and realized that the same process of heat treating blood products of other animals could treat humans with diphtheria.[18] By 1896, the introduction of diphtheria antitoxin was hailed as "the most important advance of the [19th] Century in the medical treatment of acute infective disease".[19]
Prior to the advent of vaccines and antibiotics, specific antitoxin was often the only treatment available for infections such as diphtheria and tetanus. Immunoglobulin therapy continued to be a first line therapy in the treatment of severe respiratory diseases until the 1930s, even after sulfonamides were introduced.[13]

In 1890 antibody therapy was used to treat tetanus, when serum from immunized horses was injected into patients with severe tetanus in an attempt to neutralize the tetanus toxin, and prevent the dissemination of the disease. Since the 1960s, human tetanus immune globulin (TIG) has been used in the United States in unimmunized, vaccine-naive or incompletely immunized patients who have sustained wounds consistent with the development of tetanus.[13] The administration of horse antitoxin remains the only specific pharmacologic treatment available for botulism.[20] Antitoxin also known as heterologous hyperimmune serum is often also given prophylactically to individuals known to have ingested contaminated food.[6] IVIG treatment was also used successfully to treat several patients with toxic shock syndrome, during the 1970s tampon scare.[citation needed]
Antibody therapy is also used to treat viral infections. In 1945, hepatitis A infections, epidemic in summer camps, were successfully prevented by immunoglobulin treatment. Similarly, hepatitis B immune globulin (HBIG) effectively prevents hepatitis B infection. Antibody prophylaxis of both hepatitis A and B has largely been supplanted by the introduction of vaccines; however, it is still indicated following exposure and prior to travel to areas of endemic infection.[21]
In 1953, human vaccinia immunoglobulin (VIG) was used to prevent the spread of smallpox during an outbreak in Madras, India, and continues to be used to treat complications arising from smallpox vaccination. Although the prevention of measles is typically induced through vaccination, it is often treated immuno-prophylactically upon exposure. Prevention of rabies infection still requires the use of both vaccine and immunoglobulin treatments.[13]
During a 1995 Ebola virus outbreak in the Democratic Republic of Congo, whole blood from recovering patients, and containing anti-Ebola antibodies, was used to treat eight patients, as there was no effective means of prevention, though a treatment was discovered recently in the 2013 Ebola epidemic in Africa. Only one of the eight infected patients died, compared to a typical 80% Ebola mortality, which suggested that antibody treatment may contribute to survival.[22] Immune globulin or immunoglobulin has been used to both prevent and treat reactivation of the herpes simplex virus (HSV), varicella zoster virus, Epstein-Barr virus (EBV), and cytomegalovirus (CMV).[13]
FDA licensed immunoglobulins
[edit]The following immunoglobulins are the immunoglobulins currently approved for use for infectious disease prophylaxis and immunotherapy, in the United States.[23]
| Disease | Product[a] | Source | Use |
|---|---|---|---|
| Botulism | Specific equine IgG | horse | Treatment of wound and food borne forms of botulism. |
| Despeciated equine IgG[24] | |||
| Human specific IgG[24] | human | Treatment of infant botulism types A and B; brand name "BabyBIG". | |
| Cytomegalovirus (CMV) | hyperimmune IVIG | human | Prophylaxis, used most often in kidney transplant patients. |
| Diphtheria | Specific equine IgG | horse | Treatment of diphtheria infection. |
| Hepatitis B | Hepatitis B Ig | human | Post-exposure prophylaxis, prevention in high-risk infants (administered with Hepatitis B vaccine). |
| Hepatitis A, measles | Pooled human Ig | human serum | Prevention of Hepatitis A and measles infection, treatment of congenital or acquired immunodeficiency. |
| ITP, Kawasaki disease, IgG deficiency |
Pooled human IgG | human serum | Treatment of ITP and Kawasaki disease, prevention/treatment of opportunistic infection with IgG deficiency. |
| Rabies | Rabies Ig | human | Post-exposure prophylaxis (administered with rabies vaccine). |
| Tetanus | Tetanus Ig | human | Treatment of tetanus infection. |
| Vaccinia | Vaccinia Ig | human | Treatment of progressive vaccinia infection including eczema and ocular forms (usually resulting from smallpox vaccination in immunocompromised individuals). |
| Varicella (chicken-pox) | Varicella-zoster Ig | human | Post-exposure prophylaxis in high risk individuals. |
| Rh disease | Rho(D) immune globulin | human | Prevention of RhD isoimmunization in Rh(D)-negative mothers[25] |
- ^ Specific or not noted: hyperimmune globulin or antitoxin. Pooled: mixed Ig from ordinary sources, also known as normal human immunoglobulin.
Passive transfer of cell-mediated immunity
[edit]The one exception to passive humoral immunity is the passive transfer of cell-mediated immunity, also called adoptive immunization which involves the transfer of mature circulating lymphocytes. It is rarely used in humans, and requires histocompatible (matched) donors, which are often difficult to find, and carries severe risks of graft-versus-host disease.[2] This technique has been used in humans to treat certain diseases including some types of cancer and immunodeficiency. However, this specialized form of passive immunity is most often used in a laboratory setting in the field of immunology, to transfer immunity between "congenic", or deliberately inbred mouse strains which are histocompatible.[citation needed]
Advantages and disadvantages
[edit]Passive immunity starts working faster than vaccines do, as the patient's immune system does not need to make its own antibodies: B cells take time to activate and multiply after a vaccine is given. Passive immunity works even if an individual has a immune system disorder that prevents them from making antibodies in response to a vaccine.[18] In addition to conferring passive immunities, breastfeeding has other lasting beneficial effects on the baby's health, such as decreased risk of allergies and obesity.[26]
A disadvantage to passive immunity is that producing antibodies in a laboratory is expensive and difficult to do. In order to produce antibodies for infectious diseases, there is a need for possibly thousands of human donors to donate blood or immune animals' blood would be obtained for the antibodies. Patients who are immunized with the antibodies from animals may develop serum sickness due to the proteins from the immune animal and develop serious allergic reactions.[6] Antibody treatments can be time-consuming and are given through an intravenous injection or IV, while a vaccine shot or jab is less time-consuming and has less risk of complication than an antibody treatment. Passive immunity is effective, but only lasts a short amount of time.[18]
See also
[edit]References
[edit]- ^ "Vaccines: Vac-Gen/Immunity Types". www.cdc.gov. Archived from the original on 2011-12-22. Retrieved 2015-11-20.
- ^ a b c "Microbiology/Virology/Immunology/Bacteriology/Parasitology Text Book On-line". www.microbiologybook.org. Archived from the original on 2021-05-30. Retrieved 2023-09-28.
- ^ "Passive Immunization - Infectious Diseases". Merck Manuals Professional Edition. Archived from the original on 2020-04-08. Retrieved 2015-11-12.
- ^ Kalenik, Barbara; Sawicka, Róża; Góra-Sochacka, Anna; Sirko, Agnieszka (2014-01-01). "Influenza prevention and treatment by passive immunization". Acta Biochimica Polonica. 61 (3): 573–587. doi:10.18388/abp.2014_1879. ISSN 1734-154X. PMID 25210721.
- ^ Lambert, Paul-Henri; Liu, Margaret; Siegrist, Claire-Anne (April 2005). "Can successful vaccines teach us how to induce efficient protective immune responses?". Nature Medicine. 11 (4): S54–S62. doi:10.1038/nm1216. ISSN 1546-170X. Archived from the original on 2017-05-09. Retrieved 2023-09-28.
- ^ a b c d "Centers for Disease Control and Prevention" (PDF). Archived (PDF) from the original on 2020-04-08. Retrieved 2017-09-07.
- ^ a b c Janeway, Charles; Paul Travers; Mark Walport; Mark Shlomchik (2001). Immunobiology; Fifth Edition. New York and London: Garland Science. ISBN 0-8153-4101-6. Archived from the original on 2009-06-28. Retrieved 2017-09-07..
- ^ "WHO | Exclusive breastfeeding". www.who.int. Archived from the original on 2019-10-30. Retrieved 2016-06-06.
- ^ Mestecky, Jiri; Strober, Warren; Russell, Michael W.; Cheroutre, Hilde; Lambrecht, Bart N.; Kelsall, Brian L. (15 April 2015). Mucosal Immunology. ISBN 9780124158474.
- ^ Kedl, Ross M.; Hsieh, Elena W. Y.; Morrison, Thomas E.; Samayoa-Reyes, Gabriela; Flaherty, Siobhan; Jackson, Conner L.; Rochford, Rosemary (2023). "Evidence for Aerosol Transfer of SARS-CoV-2–Specific Humoral Immunity". pp. 307–309. medRxiv 10.1101/2022.04.28.22274443.
- ^ Sheikh-Mohamed, Salma; Isho, Baweleta; Chao, Gary Y. C.; Zuo, Michelle; Cohen, Carmit; Lustig, Yaniv; Nahass, George R.; Salomon-Shulman, Rachel E.; Blacker, Grace; Fazel-Zarandi, Mahya; Rathod, Bhavisha; Colwill, Karen; Jamal, Alainna; Li, Zhijie; de Launay, Keelia Quinn; Takaoka, Alyson; Garnham-Takaoka, Julia; Patel, Anjali; Fahim, Christine; Paterson, Aimee; Li, Angel Xinliu; Haq, Nazrana; Barati, Shiva; Gilbert, Lois; Green, Karen; Mozafarihashjin, Mohammad; Samaan, Philip; Budylowski, Patrick; Siqueira, Walter L.; Mubareka, Samira; Ostrowski, Mario; Rini, James M.; Rojas, Olga L.; Weissman, Irving L.; Tal, Michal Caspi; McGeer, Allison; Regev-Yochay, Gili; Straus, Sharon; Gingras, Anne-Claude; Gommerman, Jennifer L. (25 April 2022). "Systemic and mucosal IgA responses are variably induced in response to SARS-CoV-2 mRNA vaccination and are associated with protection against subsequent infection". Mucosal Immunology. 15 (5): 799–808. doi:10.1038/s41385-022-00511-0. ISSN 1935-3456. PMC 9037584. PMID 35468942. S2CID 248389239.
- ^ "prophylactically". Archived from the original on 2020-04-08. Retrieved 2015-11-20.
{{cite journal}}: Cite journal requires|journal=(help) - ^ a b c d e Keller, Margaret A.; Stiehm, E. Richard (1 October 2000). "Passive Immunity in Prevention and Treatment of Infectious Diseases". Clinical Microbiology Reviews. 13 (4): 602–614. doi:10.1128/cmr.13.4.602. PMC 88952. Archived from the original on 28 September 2023. Retrieved 28 September 2023.
- ^ "Types of Immunity to a Disease | CDC". www.cdc.gov. 2022-04-06. Archived from the original on 2011-12-22. Retrieved 2023-09-28.
- ^ Baxter, David (2007-12-01). "Active and passive immunity, vaccine types, excipients and licensing". Occupational Medicine. 57 (8): 552–556. doi:10.1093/occmed/kqm110. ISSN 0962-7480. PMID 18045976.
- ^ Dolman, C.E. (1973). "Landmarks and pioneers in the control of diphtheria". Can. J. Public Health. 64 (4): 317–36. PMID 4581249.
- ^ Silverstein, Arthur M. (1989) History of Immunology (Hardcover) Academic Press. Note: The first six pages of this text are available online at: (Amazon.com easy reader Archived 2020-04-08 at the Wayback Machine)
- ^ a b c "Passive Immunization — History of Vaccines". www.historyofvaccines.org. Archived from the original on 2020-04-08. Retrieved 2015-11-20.
- ^ (Report) (1896). "Report of the Lancet Special Commission on the relative strengths of diphtheria antitoxic serums". Lancet. 148 (3803): 182–95. doi:10.1016/s0140-6736(01)72399-9. PMC 5050965.
- ^ Shapiro, R. L.; Hatheway, C.; Swerdlow, D. L. (1998-08-01). "Botulism in the United States: a clinical and epidemiologic review". Annals of Internal Medicine. 129 (3): 221–228. doi:10.7326/0003-4819-129-3-199808010-00011. ISSN 0003-4819. PMID 9696731. Archived from the original on 2022-10-09. Retrieved 2023-09-29.
- ^ Casadevall, A., and M. D. Scharff. 1995. Return to the past: the case for antibody-based therapies in infectious diseases. Clin. Infect. Dis. 21:150-161
- ^ Mupapa, K., M. Massamba, K. Kibadi, K. Kivula, A. Bwaka, M. Kipasa, R. Colebunders, and J. J. Muyembe-Tamfum on behalf of the International Scientific and Technical Committee. 1999. Treatment of Ebola hemorrhagic fever with blood transfusions from convalescent patients. J. Infect. Dis. 179(Suppl.):S18-S23
- ^ Robbins, John B.; Schneerson, Rachel; Szu, Shousun C. (1996). "Table 8-2, U.S. Licensed Immunoglobulin For Passive Immunization". www.ncbi.nlm.nih.gov. Archived from the original on 2013-12-05. Retrieved 2023-09-29.
- ^ a b Stanek, Scott A.; Saunders, David; Alves, Derron A. (2020). USAMRIID's Medical Management of Biological Casualties Handbook (PDF) (9th ed.). U.S. Army Medical Research Institute of Infectious Diseases. ISBN 978-0-16-095526-6.
- ^ "Rho(D) Immune Globulin". Drugs.com. The American Society of Health-System Pharmacists. Archived from the original on 9 January 2017. Retrieved 8 January 2017.
- ^ "Breastfeeding Overview". WebMD. Archived from the original on 2020-04-08. Retrieved 2015-11-20.
