Portal:Viruses
The Viruses Portal
Welcome!
Viruses are small infectious agents that can replicate only inside the living cells of an organism. Viruses infect all forms of life, including animals, plants, fungi, bacteria and archaea. They are found in almost every ecosystem on Earth and are the most abundant type of biological entity, with millions of different types, although only about 6,000 viruses have been described in detail. Some viruses cause disease in humans, and others are responsible for economically important diseases of livestock and crops.
Virus particles (known as virions) consist of genetic material, which can be either DNA or RNA, wrapped in a protein coat called the capsid; some viruses also have an outer lipid envelope. The capsid can take simple helical or icosahedral forms, or more complex structures. The average virus is about 1/100 the size of the average bacterium, and most are too small to be seen directly with an optical microscope.
The origins of viruses are unclear: some may have evolved from plasmids, others from bacteria. Viruses are sometimes considered to be a life form, because they carry genetic material, reproduce and evolve through natural selection. However they lack key characteristics (such as cell structure) that are generally considered necessary to count as life. Because they possess some but not all such qualities, viruses have been described as "organisms at the edge of life".
Selected disease
Gastroenteritis is an inflammation of the gastrointestinal tract involving both the stomach and small intestine, which results in diarrhoea and vomiting, and sometimes abdominal pain. It is usually caused by a virus: most commonly rotavirus and norovirus, but also adenovirus and astrovirus. Other major infectious causes include Campylobacter, Escherichia coli, Vibrio cholerae and some other bacteria, as well as protozoa. Viruses, particularly rotavirus, cause about 70% of gastroenteritis episodes in children, while norovirus is the leading cause of gastroenteritis among adults in America, causing over 90% of outbreaks.
Transmission can be from consumption of improperly prepared foods or contaminated water, or by close contact with infectious individuals. Good sanitation practices and a convenient supply of uncontaminated water are important for reducing infection. Personal measures such as hand washing with soap can decrease incidence by as much as 30%. An estimated 2 billion cases of gastroenteritis occurred globally in 2015, mainly among children and people in developing countries, resulting in 1.3 million deaths. Gastroenteritis is usually an acute and self-limiting disease that does not require medication; the main treatment is rehydration using oral rehydration therapy. A rotavirus vaccine is available.
Selected image
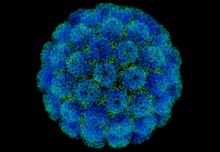
Chikungunya virus is an alphavirus transmitted by Aedes mosquitoes. The disease can cause severe joint pain, sometimes lasting for several months. Outbreaks have occurred across Africa, Asia and India, and in 2013–14, in South America and the Caribbean.
Credit: A2-33 (8 December 2013)
In the news
26 February: In the ongoing pandemic of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), more than 110 million confirmed cases, including 2.5 million deaths, have been documented globally since the outbreak began in December 2019. WHO
18 February: Seven asymptomatic cases of avian influenza A subtype H5N8, the first documented H5N8 cases in humans, are reported in Astrakhan Oblast, Russia, after more than 100,0000 hens died on a poultry farm in December. WHO
14 February: Seven cases of Ebola virus disease are reported in Gouécké, south-east Guinea. WHO
7 February: A case of Ebola virus disease is detected in North Kivu Province of the Democratic Republic of the Congo. WHO
4 February: An outbreak of Rift Valley fever is ongoing in Kenya, with 32 human cases, including 11 deaths, since the outbreak started in November. WHO
21 November: The US Food and Drug Administration (FDA) gives emergency-use authorisation to casirivimab/imdevimab, a combination monoclonal antibody (mAb) therapy for non-hospitalised people twelve years and over with mild-to-moderate COVID-19, after granting emergency-use authorisation to the single mAb bamlanivimab earlier in the month. FDA 1, 2
18 November: The outbreak of Ebola virus disease in Équateur Province, Democratic Republic of the Congo, which started in June, has been declared over; a total of 130 cases were recorded, with 55 deaths. UN
Selected article
Viruses and viral infections have affected human history. Epidemics caused by viruses began when human behaviour changed during the Neolithic period, around 12,000 years ago. Previously hunter-gatherers, humans developed more densely populated agricultural communities, which allowed viruses to spread rapidly and subsequently to become endemic. Viruses of plants and livestock also increased, and as humans became dependent on agriculture and farming, diseases such as potyviruses of potatoes and rinderpest of cattle had devastating consequences. Smallpox and measles viruses are among the oldest that infect humans. They first appeared in humans in Europe and North Africa thousands of years ago, having evolved from viruses that infected other animals. Influenza pandemics have been recorded since 1580.
There are an estimated 1031 viruses on Earth. Although scientific interest in them arose because of the diseases they cause, most viruses are beneficial. They drive evolution by transferring genes across species, play important roles in ecosystems, and are essential to life.
Selected outbreak
The 1976 Zaire Ebola virus outbreak was one of the first two recorded outbreaks of the disease. The causative agent was identified as a novel virus, named for the region's Ebola River. The first identified case, in August, worked in the school in Yambuku, a small rural village in Mongala District, north Zaire. He had been treated for suspected malaria at the Yambuku Mission Hospital, which is now thought to have spread the virus by giving vitamin injections with inadequately sterilised needles, particularly to women attending prenatal clinics. Unsafe burial practices also spread the virus.
The outbreak was contained by quarantining local villages, sterilising medical equipment and providing protective clothing to medical personnel, and was over by early November. A total of 318 cases was recorded, of whom 280 died, an 88% case fatality rate. An earlier outbreak in June–November in Nzara, Sudan, was initially thought to be linked, but was shown to have been caused by a different species of Ebola virus.
Selected quotation
| “ | To help conceptualize the sheer number of viruses in existence, their current biomass has been estimated to equal that of 75 million blue whales (approximately 200 million tonnes) and, if placed end to end, the collective length of their virions would span 65 galaxies. | ” |
—Peter Simmonds
Recommended articles
Viruses & Subviral agents: bat virome • elephant endotheliotropic herpesvirus • HIV • introduction to viruses![]() • Playa de Oro virus • poliovirus • prion • rotavirus
• Playa de Oro virus • poliovirus • prion • rotavirus![]() • virus
• virus![]()
Diseases: colony collapse disorder • common cold • croup • dengue fever![]() • gastroenteritis • Guillain–Barré syndrome • hepatitis B • hepatitis C • hepatitis E • herpes simplex • HIV/AIDS • influenza
• gastroenteritis • Guillain–Barré syndrome • hepatitis B • hepatitis C • hepatitis E • herpes simplex • HIV/AIDS • influenza![]() • meningitis
• meningitis![]() • myxomatosis • polio
• myxomatosis • polio![]() • pneumonia • shingles • smallpox
• pneumonia • shingles • smallpox
Epidemiology & Interventions: 2007 Bernard Matthews H5N1 outbreak • Coalition for Epidemic Preparedness Innovations • Disease X • 2009 flu pandemic • HIV/AIDS in Malawi • polio vaccine • Spanish flu • West African Ebola virus epidemic
Virus–Host interactions: antibody • host • immune system![]() • parasitism • RNA interference
• parasitism • RNA interference![]()
Methodology: metagenomics
Social & Media: And the Band Played On • Contagion • "Flu Season" • Frank's Cock![]() • Race Against Time: Searching for Hope in AIDS-Ravaged Africa
• Race Against Time: Searching for Hope in AIDS-Ravaged Africa![]() • social history of viruses
• social history of viruses![]() • "Steve Burdick" • "The Time Is Now" • "What Lies Below"
• "Steve Burdick" • "The Time Is Now" • "What Lies Below"
People: Brownie Mary • Macfarlane Burnet![]() • Bobbi Campbell • Aniru Conteh • people with hepatitis C
• Bobbi Campbell • Aniru Conteh • people with hepatitis C![]() • HIV-positive people
• HIV-positive people![]() • Bette Korber • Henrietta Lacks • Linda Laubenstein • Barbara McClintock
• Bette Korber • Henrietta Lacks • Linda Laubenstein • Barbara McClintock![]() • poliomyelitis survivors
• poliomyelitis survivors![]() • Joseph Sonnabend • Eli Todd • Ryan White
• Joseph Sonnabend • Eli Todd • Ryan White![]()
Selected virus
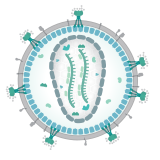
Human immunodeficiency virus (HIV) is a lentivirus, an RNA virus in the retrovirus family. Two types of HIV have been characterised: HIV-1 is the more virulent and is responsible for most infections worldwide; HIV-2 is mainly confined to West Africa. The genome consists of two copies of a single-stranded +RNA, which contains nine genes. The roughly spherical virus particle has a diameter of about 120 nm; it is enveloped and contains a conical capsid made of around 2,000 copies of the p24 protein. The envelope glycoprotein, a trimeric complex of gp120 and gp41, binds to CD4, the primary receptor on the host cell.
Transmission occurs by the transfer of bodily fluids including blood, semen, vaginal fluids and breast milk, in which the virus is present both as free virus particles and within infected immune cells. HIV infects key cells in the human immune system including CD4+ T helper cells, macrophages and dendritic cells. Infection leads to low levels of CD4+ T cells via several mechanisms, resulting in a progressive immunodeficiency disease known as AIDS.
Did you know?
- ...that the elegant rice rat (pictured; top) sometimes carries a hantavirus that can cause a fatal disease in humans?
- ...that a quaranjavirus that can infect humans was discovered in 1953, but it took 60 years to classify it?
- ...that in 1918, infected crew members aboard HMS Mantua inadvertently spread the Spanish flu to Africa?
- ...that in the mid-1980s, some HIV patients pinned their hopes for survival on an experimental drug called HPA-23?
- ...that Li Zaiping and his research group were the first to sequence a viral genome in China?
Selected biography
Peter Piot (born 17 February 1949) is a Belgian virologist and public health specialist, known for his work on Ebola virus and HIV.
During the first outbreak of Ebola in Yambuku, Zaire in 1976, Piot was one of a team that discovered the filovirus in a blood sample. He and his colleagues travelled to Zaire to help to control the outbreak, and showed that the virus is transmitted via blood and during preparation of bodies for burial. He advised WHO during the West African Ebola epidemic of 2014–16.
In the 1980s, Piot participated in collaborative projects in Burundi, Côte d'Ivoire, Kenya, Tanzania and Zaire, including Project SIDA in Kinshasa, the first international project on AIDS in Africa, which provided the foundations for understanding HIV infection in that continent. He was the founding director of UNAIDS, and has served as president of the International AIDS Society and assistant director of the WHO Global HIV/AIDS Programme. As of 2020, he directs the London School of Hygiene & Tropical Medicine.
In this month
1 August 1971: The term viroid was coined by Theodor Diener to describe the agent of potato spindle tuber disease
6 August 2007: Maraviroc, first CCR5 receptor antagonist, approved for HIV/AIDS
8 August 2011: UN declared rinderpest eradicated
8 August 2014: WHO declared the Ebola outbreak in West Africa (virus pictured), the most widespread so far, an international public health emergency
18 August 1990: Ryan White Care Act enacted, the largest American federally funded programme for people living with HIV/AIDS
20 August 1780: Start of an outbreak of dengue fever in Philadelphia, USA, which led Benjamin Rush to describe the disease in 1789
26 August 1976: First case of Ebola virus, now the Zaire form
26 August 1998: Fomivirsen, first antisense drug, approved for cytomegalovirus retinitis
Selected intervention
Ribavirin is a nucleoside analogue that mimics the nucleoside guanosine. It shows some activity against a broad range of DNA and RNA viruses, but is less effective against dengue fever, yellow fever and other flaviviruses. The drug was first synthesised in the early 1970s by Joseph T. Witkowski and Roland K. Robins. Ribavirin's main current use is against hepatitis C, in combination with pegylated interferon, nucleotide analogues and protease inhibitors. It has been used in the past in an aerosol formulation against respiratory syncytial virus-related diseases in children. Ribavirin has been used in combination as part of an experimental treatment for rabies. It is also the only available treatment for the viruses causing some viral haemorrhagic fevers, including Lassa fever, Crimean–Congo haemorrhagic fever and hantavirus disease, but is ineffective against the filovirus diseases, Ebola and Marburg. Clinical use is limited by the drug building up in red blood cells to cause haemolytic anaemia.
Subcategories
Subcategories of virology:
Topics
Things to do
- Comment on what you like and dislike about this portal
- Join the Viruses WikiProject
- Tag articles on viruses and virology with the project banner by adding {{WikiProject Viruses}} to the talk page
- Assess unassessed articles against the project standards
- Create requested pages: red-linked viruses | red-linked virus genera
- Expand a virus stub into a full article, adding images, citations, references and taxoboxes, following the project guidelines
- Create a new article (or expand an old one 5-fold) and nominate it for the main page Did You Know? section
- Improve a B-class article and nominate it for Good Article
 or Featured Article
or Featured Article status
status - Suggest articles, pictures, interesting facts, events and news to be featured here on the portal
WikiProjects & Portals
 WikiProject Viruses
Related WikiProjects
WikiProject Viruses
Related WikiProjects
Medicine • Microbiology • Molecular & Cellular Biology • Veterinary Medicine
Related PortalsAssociated Wikimedia
The following Wikimedia Foundation sister projects provide more on this subject:
-
Commons
Free media repository -
Wikibooks
Free textbooks and manuals -
Wikidata
Free knowledge base -
Wikinews
Free-content news -
Wikiquote
Collection of quotations -
Wikisource
Free-content library -
Wikispecies
Directory of species -
Wikiversity
Free learning tools -
Wiktionary
Dictionary and thesaurus