Treponema pallidum
| Treponema pallidum | |
|---|---|
| |
| Scientific classification | |
| Domain: | Bacteria |
| Phylum: | Spirochaetota |
| Class: | Spirochaetia |
| Order: | Spirochaetales |
| Family: | Treponemataceae |
| Genus: | Treponema |
| Species: | T. pallidum
|
| Binomial name | |
| Treponema pallidum | |
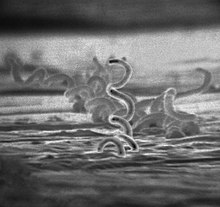
Treponema pallidum, formerly known as Spirochaeta pallida, is a microaerophilic, gram-negative, spirochaete bacterium with subspecies that cause the diseases syphilis, bejel (also known as endemic syphilis), and yaws.[1] It is known to be transmitted only among humans and baboons.[2] T. pallidum can enter the host through mucosal membranes or open lesions in the skin and is primarily spread through sexual contact.[3] It is a helically coiled microorganism usually 6–15 μm long and 0.1–0.2 μm wide. T. pallidum's lack of both a tricarboxylic acid cycle and processes for oxidative phosphorylation results in minimal metabolic activity.[4] As a chemoorganoheterotroph, Treponema pallidum is an obligate parasite that acquires its glucose carbon source from its host. Glucose can be used not only as a primary carbon source but also in glycolytic mechanisms to generate ATP needed to power the bacterium given its minimal genome.[5] The treponemes have cytoplasmic and outer membranes. Using light microscopy, treponemes are visible only by using dark-field illumination. T. pallidum consists of three subspecies, T. p. pallidum, T. p. endemicum, and T. p. pertenue, each of which has a distinct related disorder. The ability of T. pallidum to avoid host immune defenses has allowed for stealth pathogenicity.[6] The unique outer membrane structure and minimal expression of surface proteins of T. pallidum has made vaccine development difficult. Treponema pallidum can be treated with high efficacy by antibiotics that inhibit bacterial cell wall synthesis such as the beta-lactam antimicrobial penicillin-G.[7]
Subspecies
[edit]Three subspecies of T. pallidum are known:[8]
- Treponema pallidum pallidum, which causes syphilis
- T. p. endemicum, which causes bejel or endemic syphilis
- T. p. pertenue, which causes yaws
The three subspecies causing yaws, bejel, and syphilis are morphologically and serologically indistinguishable.[9] The three subspecies can be distinguished by genetics, using restriction fragment length polymorphism (RFLP), which utilizes techniques such as PCR, restriction digest and gel electrophoresis.[10] Genes TprC, TprI, and the 5' flanking region of tpp15 can be used to differentiate between the three subspecies based on DNA fragment lengths and location of bands in gel electrophoresis.[11][12] These bacteria were originally classified as members of separate species, but DNA hybridization analysis indicates they are members of the same species. Treponema carateum, the cause of pinta, remains a separate species because no isolate is available for DNA analysis.[13] Disease transmittance in subspecies T. p. endemicum and T. p. pertenue is considered non-venereal.[14] T. p. pallidum is the most invasive pathogenic subspecies, while T. carateum is the least invasive of the species. T. p. endemicum and T. p. pertenue are intermediately invasive.[9]
Laboratory identification
[edit]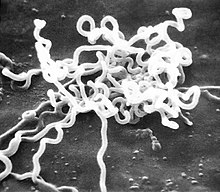
Treponema pallidum was first microscopically identified in syphilitic chancres by Fritz Schaudinn and Erich Hoffmann at the Charité in Berlin in 1905.[15] This bacterium can be detected with special stains, such as the Dieterle stain. T. pallidum is also detected by serology, including nontreponemal VDRL, rapid plasma reagin, treponemal antibody tests (FTA-ABS), T. pallidum immobilization reaction, and syphilis TPHA test.[16]
Microbiology
[edit]Physiology
[edit]
Treponema pallidum is a helically shaped bacterium with high motility consisting of an outer membrane, peptidoglycan layer, inner membrane, protoplasmic cylinder, and periplasmic space.[9] It is often described as gram-negative, but its outer membrane lacks lipopolysaccharide, which is found in the outer membrane of other gram-negative bacteria.[17] It has an endoflagellum (periplasmic flagellum) consisting of four main polypeptides, a core structure, and a sheath.[18] The flagellum is located within the periplasmic space and wraps around the protoplasmic cylinder. The peptidoglycan layer interacts with the endoflagellum which may aid in motility.[19] T. pallidum's outer membrane has the most contact with host cells and contains few transmembrane proteins, limiting antigenicity, while its cytoplasmic membrane is covered in lipoproteins.[20][21] The outer membrane's treponemal ligands' main function is attachment to host cells, with functional and antigenic relatedness between ligands.[22] The genus Treponema has ribbons of cytoskeletal cytoplasmic filaments that run the length of the cell just underneath the cytoplasmic membrane.
Outer membrane
[edit]The outer membrane (OM) of T. pallidum has several features that have made it historically difficult to research. These include details such as its low protein content, its fragility, and that it contains fewer gene sequences related to other gram negative outer membranes.[23] Progress has been made using genomic sequencing and advanced computational models. The treponemal outer membrane proteins are key factors for the bacterium's pathogenesis, persistence, and immune evasion strategies. The relatively low protein content prevents antigen recognition by the immune system and the proteins that do exist protrude out of the OM, enabling its interaction with the host.[23] Treponema's reputation as a "stealth pathogen" is primarily due to this unique OM structure, which serves to evade immune detection.[23]
TP0126
[edit]The TP0126 protein has been linked to the outer membrane protein family (OMP). This protein will sit in the outer membrane like a porin, which is supported by circular dichroism recombinant TP0126, and will increase the virulence factor.[24] Researchers have classified the TP0126 protein in this class due to the homology between the protein and the porins of the OMPs.[25][24] This protein is encoded by the tp0126 gene, which is conserved over all strains of T. pallidum. [25]
TP0326
[edit]TP0326 is an ortholog of the β-barrel assembly machine Bam A. BamA apparatus inserts newly synthetized and exported outer membrane proteins into the outer membrane.[26]
TP0453
[edit]TP0453 is a 287 amino acid protein associated with the inner membrane of the microbe's outer membrane.[27] This protein lacks the extensive beta sheet structure that is characteristic of other membrane proteins, and does not traverse the outer membrane.[28] This protein's function has been hypothesized to be involved with control of nutrient uptake.[29]
TP0624
[edit]Outer Membrane Protein A (OmpA) domain-containing proteins are necessary for maintaining structural integrity in gram-negative bacteria. These domains contain peptidoglycan binding sites which creates a "structural bridge between the peptidoglycan layer and the outer memebrane."[30] The protein TP0624 found in T. pallidum has been proposed to facilitate this structural link, as well as interactions between outer membrane proteins and corresponding domains on the thin peptidoglycan layer.[30]
TP0751
[edit]The TP0751 protein is a protein that is unique to T. pallidum, and it is thought to aid in attachment to the host's extra cellular membrane.[31] Since this protein aids in the attachment to the host, it sits on the surface of the cells, and in 2005, it was discovered that the TP0751 protein will attach to the laminin component in the host's extracellular matrix.[32] With that, it is thought that the TP0751 protein plays a key role in dissemination with the host.[32][31]
TP0965
[edit]TP0965 is a protein that is critical for membrane fusion in T. pallidum, and is located in the periplasm.[27] TP0965 causes endothelial barrier dysfunction, a hallmark of late-stage pathogenesis of syphilis.[33] It does this by reducing the expression of tight junction proteins, which in turn increases the expression of adhesion molecules and endothelial cell permeability, which eventually leads to disruption of the endothelial layer.[34]
Treponema repeat family of proteins
[edit]The Treponema repeat family of proteins (Tpr) are proteins expressed during the infection process. Tprs are formed by a conserved N-terminal domain, an amino-terminal stretch of about 50 amino acids, a central variable region, and a conserved C-terminal domain.[26] The many different types of Tpr include TprA, TprB, TprC, TprD, and TprE, but variability of TprK is the most relevant due to the immune escape characteristics it allows.[35]
Antigen variation in TprK is regulated by gene conversion. In this way, fragments of the seven variable regions (V1–V7), by nonreciprocal recombination, present in TprK and the 53 donor sites of TprD can be combined to produce new structured sequences.[36][37] TprK antigen variation can help T. pallidum to evade a strong host immune reaction and can also allow the reinfection of individuals. This is possible because the newly structured proteins can avoid antibody-specific recognition.[35] This is possible because the newly structured proteins can avoid antibody-specific recognition. It is also suspected that the genes that encode for the TprK protein are essential in pathogenesis during the infection of syphilis.[35]
To introduce more phenotypic diversity, T. pallidum may undergo phase variation. This process mainly happens in TprF, TprI, TprG, TprJ, and TprL, and it consists of a reversible expansion or contraction of polymeric repeats. These size variations can help the bacterium to quickly adapt to its microenvironment, dodge immune response, or even increase affinity to its host.[37]
Culture
[edit]In the past century since its initial discovery, culturing the bacteria in vitro has been difficult.[38] Without the ability to grow and maintain the bacteria in a laboratory setting, discoveries regarding its metabolism and antimicrobial sensitivity were greatly impaired.[23] However, successful long-term cultivation of T. pallidum in vitro was reported in 2017.[38] This was achieved using Sf1Ep epithelial cells from rabbits, which were a necessary condition for the continued multiplication and survival of the system.[39] The medium TpCM-2 was used, an alteration of more simple media which previously only yielded a few weeks of culture growth.[39] This success was the result of switching out minimal essential medium (MEM) with CMRL 1066, a complex tissue culture medium.[38] With development, new discoveries about T. pallidum's requirements for growth and gene expression may occur and in turn, yield research beneficial for the treatment and prevention of syphilis, outside of a host.[40] However, continuous efforts to grow T. pallidum in axenic culture have been unsuccessful, indicating that it does not satisfy Koch's postulates.[41] The challenge likely stems from the organism's strong adaptation to residing in mammalian tissue, resulting in a reduced genome and significant impairments in metabolic and biosynthetic functions.[39]
Genome
[edit]The genome of T. pallidum was first sequenced in 1998.[42] It is characterized by its helical, corkscrew-like shape.[43] T. pallidum is not obtainable in a pure culture, meaning that this sequencing played an important role in filling gaps of understanding regarding the microbes' functions. The DNA sequences of T. pallidum species are more than 99.7% identical, and PCR-based assays are effective at differentiating these species.[44][45] About 92.9% of DNA was determined to be open reading frames, 55% of which had predicted biological functions.[20] T. pallidum was found to rely on its host for many molecules typically provided by biosynthetic pathways, and it is missing genes responsible for encoding key enzymes in oxidative phosphorylation and the tricarboxylic acid cycle.[46] The T. pallidum group and its reduced genome is likely the result of various adaptations, such that it no longer contains the ability to synthesize fatty acids, nucleic acids, and amino acids, instead relying on its mammalian hosts for these materials.[40] The recent sequencing of the genomes of several spirochetes permits a thorough analysis of the similarities and differences within this bacterial phylum and within the species.[47][48][49] The chromosomes of the T. pallidum species are small, about 1.14 Mbp. It has one of the smallest bacterial genomes and has limited metabolic capabilities, reflecting its adaptation through genome reduction to the rich environment of mammalian tissue. It conserves almost 99.8% of its small genome, and uses its constantly mutating protein TprK to avoid immune response from its host.[50] To avoid antibodies attacking it, the cell has few proteins exposed on the outer membrane sheath.[51] Its chromosome is about 1000 kilobase pairs and is circular with a 52.8% G + C average.[42] Sequencing has revealed a bundle of 12 proteins and some putative hemolysins are potential virulence factors of T. pallidum.[52] These virulence factors are thought to contribute to the bacterium's ability to evade the immune system and cause disease.[52]
Clinical significance
[edit]The clinical features of syphilis, yaws, and bejel occur in multiple stages that affect the skin. The skin lesions observed in the early stage last for weeks or months. The skin lesions are highly infectious, and the spirochetes in the lesions are transmitted by direct contact. The lesions regress as the immune response develops against T. pallidum. The latent stage that results can last a lifetime in many cases. In a few cases, the disease exits latency and enters a tertiary phase, in which destructive lesions of skin, bone, and cartilage ensue. Unlike yaws and bejels, syphilis in its tertiary stage often affects the heart, eyes, and nervous system, as well.[13]
Syphilis
[edit]Treponema pallidum pallidum is a motile spirochete that is generally acquired by close sexual contact, entering the host via breaches in squamous or columnar epithelium. The organism can also be transmitted to a fetus by transplacental passage during the later stages of pregnancy, giving rise to congenital syphilis.[53] The helical structure of T. p. pallidum allows it to move in a corkscrew motion through mucous membranes or enter minuscule breaks in the skin. In women, the initial lesion is usually on the labia, the walls of the vagina, or the cervix; in men, it is on the shaft or glans of the penis.[9] It gains access to the host's blood and lymph systems through tissue and mucous membranes. In more severe cases, it may gain access to the host by infecting the skeletal bones and central nervous system of the body.[9]
The incubation period for a T. p. pallidum infection is usually around 21 days, but can range from 10 to 90 days.[54]
Yaws
[edit]The causative agent of yaws is Treponema pallidum pertenue, which is transmissible by direct physical contact between infected people.[55] Yaws is not sexually transmitted, and occurs in tropical, humid environments of Africa, Pacific Islands, Asia and South America.[56][57] Unlike syphilis, which displays vertical transmission, one strain of T. p. pertenue researched was not vertically transmissible in a guinea pig model, and yaws cannot be spread from mother to offspring.[58][56] Yaws appears as skin lesions, usually papules, commonly on the lower extremities, but present in other areas such as the arms, trunk and hands.[59] Three stages of yaws disease have been documented: primary yaws which presents as inflamed sores on the lower body, secondary yaws which presents as a variety of skin abnormalities along with bone inflammation, and tertiary yaws, also referred to as latent yaws, which occurs when T. p. pertenue is serologically detected in the host but no clinical signs are displayed until relapse, which often occurs years later.[60][59] Yaws is treated with antibiotics such as azithromycin and benzathine penicillin-G.[61]
Bejel
[edit]Bejel is caused by Treponema pallidum endemicum and is a disease is that endemic in hot and dry climates. The transmission path has not been fully mapped, however infections are thought to be transmitted via direct contact with lesion secretions or fomites rather than by sexual transmission.[62] Bejel typically causes skin lesions, which first appear as small ulcers in the mouth, and secondary lesions that form in the oropharynx, or around the nipples of nursing women.[45] Bejel can be treated with benzathine penicillin-G.[63]
Treatment
[edit]During the early 1940s, rabbit models in combination with the drug penicillin allowed for a long-term drug treatment. These experiments established the groundwork that modern scientists use for syphilis therapy. Penicillin can inhibit T. pallidum in 6–8 hours, though the cells still remain in lymph nodes and regenerate. Penicillin is not the only drug that can be used to inhibit T. pallidum; any β-lactam antibiotics or macrolides can be used.[64] The T. pallidum strain 14 has built-in resistance to some macrolides, including erythromycin and azithromycin. Resistance to macrolides in T. pallidum strain 14 is believed to derive from a single-point mutation that increased the organism's livability.[65] Many of the syphilis treatment therapies only lead to bacteriostatic results, unless larger concentrations of penicillin are used for bactericidal effects.[64][65] Penicillin overall is the most recommended antibiotic by the Centers for Disease Control, as it shows the best results with prolonged use. It can inhibit and may even kill T. pallidum at low to high doses, with each increase in concentration being more effective.[65] The Guideline Development Group has recommended the development of a new treatment, a short course treatment that is administered orally and can cross the placental barriers in pregnant women.[66]
Vaccine
[edit]No vaccine for syphilis is available as of 2024, but doxycycline postexposure prophylaxis can be used to prevent infections.[67][68][69] The outer membrane of T. pallidum has too few surface proteins for an antibody to be effective. Efforts to develop a safe and effective syphilis vaccine have been hindered by uncertainty about the relative importance of humoral and cellular mechanisms to protective immunity,[70] and because T. pallidum outer membrane proteins have not been unambiguously identified.[71][72] In contrast, some of the known antigens are intracellular, and antibodies are ineffective against them to clear the infection.[73][74] In the last century, several prototypes have been developed, and while none of them provided protection from the infection, some prevented bacteria from disseminating to distal organs and promoted accelerated healing.[75]
References
[edit]- ^ Radolf JD, Deka RK, Anand A, Šmajs D, Norgard MV, Yang XF (10 October 2016). "Treponema pallidum, the syphilis spirochete: making a living as a stealth pathogen". Nature Reviews. Microbiology. 14 (12): 744–759. doi:10.1038/nrmicro.2016.141. ISSN 1740-1534. PMC 5106329. PMID 27721440.
- ^ "ClinicalKey". www.clinicalkey.com. Retrieved 12 November 2024.
- ^ Radolf JD (1996), Baron S (ed.), "Treponema", Medical Microbiology (4th ed.), Galveston (TX): University of Texas Medical Branch at Galveston, ISBN 978-0-9631172-1-2, PMID 21413263, retrieved 7 November 2024
- ^ Norris SJ, Cox DL, Weinstock GM (3 January 2001). "Biology of Treponema pallidum: correlation of functional activities with genome sequence data". Journal of Molecular Microbiology and Biotechnology. 3 (1): 37–62. ISSN 1464-1801. PMID 11200228.
- ^ Brautigam CA, Deka RK, Liu WZ, Norgard MV (2016). "The Tp0684 (MglB-2) Lipoprotein of Treponema pallidum: A Glucose-Binding Protein with Divergent Topology". PLOS ONE. 11 (8): e0161022. Bibcode:2016PLoSO..1161022B. doi:10.1371/journal.pone.0161022. ISSN 1932-6203. PMC 4990184. PMID 27536942.
- ^ Radolf JD, Deka RK, Anand A, Šmajs D, Norgard MV, Yang XF (December 2016). "Treponema pallidum, the syphilis spirochete: making a living as a stealth pathogen". Nature Reviews. Microbiology. 14 (12): 744–759. doi:10.1038/nrmicro.2016.141. ISSN 1740-1526. PMC 5106329. PMID 27721440.
- ^ Gartlan WA, Rahman S, Pellegrini MV, Reti K (2024), "Benzathine Penicillin", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 29939545, retrieved 12 November 2024
- ^ Marks M, Solomon AW, Mabey DC (October 2014). "Endemic treponemal diseases". Transactions of the Royal Society of Tropical Medicine and Hygiene. 108 (10): 601–7. doi:10.1093/trstmh/tru128. PMC 4162659. PMID 25157125.
- ^ a b c d e Radolf JD (1996). Baron S (ed.). Treponema (4th ed.). Galveston (TX): University of Texas Medical Branch at Galveston. ISBN 978-0-9631172-1-2. PMID 21413263. NBK7716. Retrieved 13 February 2019.
- ^ Zondag HC, Bruisten SM, Vrbová E, Šmajs D (2020). "No bejel among Surinamese, Antillean and Dutch syphilis diagnosed patients in Amsterdam between 2006-2018 evidenced by multi-locus sequence typing of Treponema pallidum isolates". PLOS ONE. 15 (3): e0230288. Bibcode:2020PLoSO..1530288Z. doi:10.1371/journal.pone.0230288. PMC 7065763. PMID 32160272.
- ^ Centurion-Lara A, Molini BJ, Godornes C, Sun E, Hevner K, Van Voorhis WC, Lukehart SA (September 2006). "Molecular differentiation of Treponema pallidum subspecies". Journal of Clinical Microbiology. 44 (9): 3377–3380. doi:10.1128/JCM.00784-06. ISSN 0095-1137. PMC 1594706. PMID 16954278.
- ^ Centurion-Lara A, Castro C, Castillo R, Shaffer JM, Van Voorhis WC, Lukehart SA (April 1998). "The flanking region sequences of the 15-kDa lipoprotein gene differentiate pathogenic treponemes". The Journal of Infectious Diseases. 177 (4): 1036–1040. doi:10.1086/515247. ISSN 0022-1899. PMID 9534979.
- ^ a b Giacani L, Lukehart SA (January 2014). "The endemic treponematoses". Clinical Microbiology Reviews. 27 (1): 89–115. doi:10.1128/CMR.00070-13. PMC 3910905. PMID 24396138.
- ^ Radolf JD (1996), Baron S (ed.), "Treponema", Medical Microbiology (4th ed.), Galveston (TX): University of Texas Medical Branch at Galveston, ISBN 978-0-9631172-1-2, PMID 21413263, retrieved 10 November 2024
- ^ Schaudinn FR, Hoffmann E (1905). "Vorläufiger Bericht über das Vorkommen von Spirochaeten in syphilitischen Krankheitsprodukten und bei Papillomen" [Preliminary report on the occurrence of Spirochaetes in syphilitic chancres and papillomas]. Arbeiten aus dem Kaiserlichen Gesundheitsamte. 22: 527–534.
- ^ Fisher B, Harvey RP, Champe PC (2007). Lippincott's Illustrated Reviews: Microbiology. Lippincott's Illustrated Reviews Series. Hagerstown, MD: Lippincott Williams & Wilkins. ISBN 978-0-7817-8215-9.
- ^ Peeling RW, Mabey D, Kamb ML, Chen XS, Radolf JD, Benzaken AS (October 2017). "Syphilis". Nature Reviews. Disease Primers. 3: 17073. doi:10.1038/nrdp.2017.73. PMC 5809176. PMID 29022569.
- ^ San Martin F, Fule L, Iraola G, Buschiazzo A, Picardeau M (1 March 2023). "Diving into the complexity of the spirochetal endoflagellum". Trends in Microbiology. 31 (3): 294–307. doi:10.1016/j.tim.2022.09.010. ISSN 0966-842X. PMID 36244923. S2CID 252916923.
- ^ Izard J, Renken C, Hsieh CE, Desrosiers DC, Dunham-Ems S, La Vake C, Gebhardt LL, Limberger RJ, Cox DL, Marko M, Radolf JD (15 December 2009). "Cryo-Electron Tomography Elucidates the Molecular Architecture of Treponema pallidum , the Syphilis Spirochete". Journal of Bacteriology. 191 (24): 7566–7580. doi:10.1128/JB.01031-09. ISSN 0021-9193. PMC 2786590. PMID 19820083.
- ^ a b Norris SJ, Cox DL, Weinstock GM (2001). "Biology of Treponema pallidum: Correlation of Functional Activities With Genome Sequence Data" (PDF). JMMB Review. 3 (1): 37–62. PMID 11200228.
- ^ Liu J, Howell JK, Bradley SD, Zheng Y, Zhou ZH, Norris SJ (November 2010). "Cellular architecture of Treponema pallidum: novel flagellum, periplasmic cone, and cell envelope as revealed by cryoelectron tomography". Journal of Molecular Biology. 403 (4): 546–61. doi:10.1016/j.jmb.2010.09.020. PMC 2957517. PMID 20850455.
- ^ Alderete JF, Baseman JB (December 1980). "Surface Characterization of Virulent Treponema pallidum". Infection and Immunity. 30 (3): 814–823. doi:10.1128/iai.30.3.814-823.1980. PMC 551388. PMID 7014451.
- ^ a b c d Radolf JD, Kumar S (2018). "The Treponema pallidum Outer Membrane". Spirochete Biology: The Post Genomic Era. Current Topics in Microbiology and Immunology. Vol. 415. pp. 1–38. doi:10.1007/82_2017_44. ISBN 978-3-319-89637-3. ISSN 0070-217X. PMC 5924592. PMID 28849315.
- ^ a b Giacani L, Brandt SL, Ke W, Reid TB, Molini BJ, Iverson-Cabral S, Ciccarese G, Drago F, Lukehart SA, Centurion-Lara A (June 2015). "Transcription of TP0126, Treponema pallidum putative OmpW homolog, is regulated by the length of a homopolymeric guanosine repeat". Infection and Immunity. 83 (6): 2275–2289. doi:10.1128/IAI.00360-15. ISSN 1098-5522. PMC 4432754. PMID 25802057.
- ^ a b Haynes AM, Godornes C, Ke W, Giacani L (August 2019). "Evaluation of the Protective Ability of the Treponema pallidum subsp. pallidum Tp0126 OmpW Homolog in the Rabbit Model of Syphilis". Infection and Immunity. 87 (8): e00323–19. doi:10.1128/IAI.00323-19. ISSN 1098-5522. PMC 6652746. PMID 31182617.
- ^ a b Hawley KL, Montezuma-Rusca JM, Delgado KN, Singh N, Uversky VN, Caimano MJ, Radolf JD, Luthra A (8 July 2021). Galperin MY (ed.). "Structural Modeling of the Treponema pallidum Outer Membrane Protein Repertoire: a Road Map for Deconvolution of Syphilis Pathogenesis and Development of a Syphilis Vaccine". Journal of Bacteriology. 203 (15): e0008221. doi:10.1128/JB.00082-21. PMC 8407342. PMID 33972353.
- ^ a b Chen J, Huang J, Liu Z, Xie Y (27 September 2022). "Treponema pallidum outer membrane proteins: current status and prospects". Pathogens and Disease. 80 (1). doi:10.1093/femspd/ftac023. PMID 35869970.
- ^ Hazlett KR, Cox DL, Decaffmeyer M, Bennett MP, Desrosiers DC, La Vake CJ, La Vake ME, Bourell KW, Robinson EJ, Brasseur R, Radolf JD (September 2005). "TP0453, a concealed outer membrane protein of Treponema pallidum, enhances membrane permeability". Journal of Bacteriology. 187 (18): 6499–6508. doi:10.1128/JB.187.18.6499-6508.2005. PMC 1236642. PMID 16159783.
- ^ Luthra A, Zhu G, Desrosiers DC, Eggers CH, Mulay V, Anand A, McArthur FA, Romano FB, Caimano MJ, Heuck AP, Malkowski MG, Radolf JD (2 December 2011). "The transition from closed to open conformation of Treponema pallidum outer membrane-associated lipoprotein TP0453 involves membrane sensing and integration by two amphipathic helices". The Journal of Biological Chemistry. 286 (48): 41656–68. doi:10.1074/jbc.M111.305284. ISSN 1083-351X. PMC 3308875. PMID 21965687.
- ^ a b Parker ML, Houston S, Wetherell C, Cameron CE, Boulanger MJ (10 November 2016). "The Structure of Treponema pallidum Tp0624 Reveals a Modular Assembly of Divergently Functionalized and Previously Uncharacterized Domains". PLOS ONE. 11 (11): e0166274. Bibcode:2016PLoSO..1166274P. doi:10.1371/journal.pone.0166274. PMC 5104382. PMID 27832149.
- ^ a b Parker ML, Houston S, Pětrošová H, Lithgow KV, Hof R, Wetherell C, Kao WC, Lin YP, Moriarty TJ, Ebady R, Cameron CE, Boulanger MJ (September 2016). "The Structure of Treponema pallidum Tp0751 (Pallilysin) Reveals a Non-canonical Lipocalin Fold That Mediates Adhesion to Extracellular Matrix Components and Interactions with Host Cells". PLOS Pathogens. 12 (9): e1005919. doi:10.1371/journal.ppat.1005919. ISSN 1553-7374. PMC 5040251. PMID 27683203.
- ^ a b Cameron CE, Brouwer NL, Tisch LM, Kuroiwa JM (November 2005). "Defining the interaction of the Treponema pallidum adhesin Tp0751 with laminin". Infection and Immunity. 73 (11): 7485–7494. doi:10.1128/IAI.73.11.7485-7494.2005. ISSN 0019-9567. PMC 1273862. PMID 16239550.
- ^ McKevitt M, Brinkman MB, McLoughlin M, Perez C, Howell JK, Weinstock GM, Norris SJ, Palzkill T (July 2005). "Genome Scale Identification of Treponema pallidum Antigens". Infection and Immunity. 73 (7): 4445–50. doi:10.1128/iai.73.7.4445-4450.2005. PMC 1168556. PMID 15972547.
- ^ Zhang RL, Zhang JP, Wang QQ (16 December 2014). "Recombinant Treponema pallidum Protein Tp0965 Activates Endothelial Cells and Increases the Permeability of Endothelial Cell Monolayer". PLOS ONE. 9 (12): e115134. Bibcode:2014PLoSO...9k5134Z. doi:10.1371/journal.pone.0115134. PMC 4267829. PMID 25514584.
- ^ a b c Centurion-Lara A, Castro C, Barrett L, Cameron C, Mostowfi M, Van Voorhis WC, Lukehart SA (15 February 1999). "Treponema pallidum major sheath protein homologue Tpr K is a target of opsonic antibody and the protective immune response". The Journal of Experimental Medicine. 189 (4): 647–656. doi:10.1084/jem.189.4.647. PMC 2192927. PMID 9989979.
- ^ Giacani L, Molini BJ, Kim EY, Godornes BC, Leader BT, Tantalo LC, Centurion-Lara A, Lukehart SA (1 April 2010). "Antigenic variation in Treponema pallidum: TprK sequence diversity accumulates in response to immune pressure during experimental syphilis". Journal of Immunology. 184 (7): 3822–3829. doi:10.4049/jimmunol.0902788. ISSN 1550-6606. PMC 3042355. PMID 20190145.
- ^ a b Tang Y, Zhou Y, He B, Cao T, Zhou X, Ning L, Chen E, Li Y, Xie X, Peng B, Hu Y, Liu S (19 October 2022). "Investigation of the immune escape mechanism of Treponema pallidum". Infection. 51 (2): 305–321. doi:10.1007/s15010-022-01939-z. PMID 36260281. S2CID 252994863.
- ^ a b c Edmondson DG, Hu B, Norris SJ (June 2018). "Long-Term in Vitro Culture of the Syphilis Spirochete Treponema pallidum subsp. pallidum". mBio. 9 (3). doi:10.1128/mBio.01153-18. PMC 6020297. PMID 29946052.
- ^ a b c Edmondson DG, DeLay BD, Kowis LE, Norris SJ (23 February 2021). "Parameters Affecting Continuous In Vitro Culture of Treponema pallidum Strains". mBio. 12 (1): 10.1128/mbio.03536–20. doi:10.1128/mbio.03536-20. PMC 8545124. PMID 33622721.
- ^ a b Edmondson DG, Norris SJ (February 2021). "In Vitro Cultivation of the Syphilis Spirochete Treponema pallidum". Current Protocols. 1 (2): e44. doi:10.1002/cpz1.44. PMC 7986111. PMID 33599121.
- ^ Prescott J, Feldmann H, Safronetz D (January 2017). "Amending Koch's postulates for viral disease: When "growth in pure culture" leads to a loss of virulence". Antiviral Research. 137: 1–5. doi:10.1016/j.antiviral.2016.11.002. PMC 5182102. PMID 27832942.
- ^ a b Fraser CM, Norris SJ, Weinstock GM, White O, Sutton GG, Dodson R, et al. (July 1998). "Complete genome sequence of Treponema pallidum, the syphilis spirochete". Science. 281 (5375): 375–88. Bibcode:1998Sci...281..375F. doi:10.1126/science.281.5375.375. PMID 9665876. S2CID 8641048.
- ^ Clark DP, Dunlap PV, Madigan JT, Martinko JM (2009). Brock Biology of Microorganisms. San Francisco: Pearson. p. 79.
- ^ Šmajs D, Strouhal M, Knauf S (July 2018). "Genetics of human and animal uncultivable treponemal pathogens". Infection, Genetics and Evolution. 61: 92–107. Bibcode:2018InfGE..61...92S. doi:10.1016/j.meegid.2018.03.015. PMID 29578082. S2CID 4826749.
- ^ a b Noda A, Grillová L, Lienhard R, Blanco O, Rodríguez I, Šmajs D (November 2018). "Bejel in Cuba: molecular identification of Treponema pallidum subsp. endemicum in patients diagnosed with venereal syphilis". Clinical Microbiology and Infection. 24 (11): 1210.e1–1210.e5. doi:10.1016/j.cmi.2018.02.006. ISSN 1198-743X. PMID 29454847.
- ^ Willey JM (2020). Prescott's Microbiology (11th ed.). McGraw-Hill Education. p. 436. ISBN 978-1-260-21188-7.
- ^ Zobaníková M, Mikolka P, Cejková D, Pospíšilová P, Chen L, Strouhal M, Qin X, Weinstock GM, Smajs D (October 2012). "Complete genome sequence of Treponema pallidum strain DAL-1". Standards in Genomic Sciences. 7 (1): 12–21. Bibcode:2012SGenS...7...12Z. doi:10.4056/sigs.2615838. PMC 3570794. PMID 23449808.
- ^ Tong ML, Zhao Q, Liu LL, Zhu XZ, Gao K, Zhang HL, Lin LR, Niu JJ, Ji ZL, Yang TC (2017). "Whole genome sequence of the Treponema pallidum subsp. pallidum strain Amoy: An Asian isolate highly similar to SS14". PLOS ONE. 12 (8): e0182768. Bibcode:2017PLoSO..1282768T. doi:10.1371/journal.pone.0182768. PMC 5546693. PMID 28787460.
- ^ Seshadri R, Myers GS, Tettelin H, Eisen JA, Heidelberg JF, Dodson RJ, et al. (April 2004). "Comparison of the genome of the oral pathogen Treponema denticola with other spirochete genomes". Proceedings of the National Academy of Sciences of the United States of America. 101 (15): 5646–51. Bibcode:2004PNAS..101.5646S. doi:10.1073/pnas.0307639101. PMC 397461. PMID 15064399.
- ^ Pinto M, Borges V, Antelo M, Pinheiro M, Nunes A, Azevedo J, Borrego MJ, Mendonça J, Carpinteiro D, Vieira L, Gomes JP (17 October 2016). "Genome-scale analysis of the non-cultivable Treponema pallidum reveals extensive within-patient genetic variation". Nature Microbiology. 2 (1): 16190. doi:10.1038/nmicrobiol.2016.190. ISSN 2058-5276. PMID 27748767.
- ^ Willey 2020, p. 499
- ^ a b Weinstock GM, Hardham JM, McLeod MP, Sodergren EJ, Norris SJ (1 October 1998). "The genome of Treponema pallidum: new light on the agent of syphilis". FEMS Microbiology Reviews. 22 (4): 323–332. doi:10.1111/j.1574-6976.1998.tb00373.x. PMID 9862125.
- ^ Arora N, Sadovsky Y, Dermody TS, Coyne CB (May 2017). "Microbial Vertical Transmission during Human Pregnancy". Cell Host Microbe. 21 (5): 561–7. doi:10.1016/j.chom.2017.04.007. PMC 6148370. PMID 28494237.
- ^ "Syphilis". www.pennmedicine.org. 10 September 2022. Retrieved 11 September 2024.
- ^ Dofitas BL, Kalim SP, Toledo CB, Richardus JH (30 January 2020). "Yaws in the Philippines: first reported cases since the 1970s". Infectious Diseases of Poverty. 9 (1): 1. doi:10.1186/s40249-019-0617-6. ISSN 2095-5162. PMC 6990502. PMID 31996251.
- ^ a b Mitjà O, Asiedu K, Mabey D (2 March 2013). "Yaws". Lancet. 381 (9868): 763–773. doi:10.1016/S0140-6736(12)62130-8. ISSN 1474-547X. PMID 23415015.
- ^ "Yaws (Endemic treponematoses)". www.who.int. Retrieved 20 November 2024.
- ^ Wicher K, Wicher V, Abbruscato F, Baughn RE (June 2000). Barbieri JT (ed.). "Treponema pallidum subsp. pertenue Displays Pathogenic Properties Different from Those of T. pallidum subsp. pallidum". Infection and Immunity. 68 (6): 3219–3225. doi:10.1128/IAI.68.6.3219-3225.2000. ISSN 0019-9567. PMC 97566. PMID 10816466.
- ^ a b Marks M, Lebari D, Solomon AW, Higgins SP (26 September 2015). "Yaws". International Journal of STD & AIDS. 26 (10): 696–703. doi:10.1177/0956462414549036. ISSN 1758-1052. PMC 4655361. PMID 25193248.
- ^ Marks M (September 2018). "Advances in the Treatment of Yaws". Tropical Medicine and Infectious Disease. 3 (3): 92. doi:10.3390/tropicalmed3030092. ISSN 2414-6366. PMC 6161241. PMID 30274488.
- ^ Mitjà O, Hays R, Ipai A, Penias M, Paru R, Fagaho D, de Lazzari E, Bassat Q (28 January 2012). "Single-dose azithromycin versus benzathine benzylpenicillin for treatment of yaws in children in Papua New Guinea: an open-label, non-inferiority, randomised trial". Lancet. 379 (9813): 342–347. doi:10.1016/S0140-6736(11)61624-3. ISSN 1474-547X. PMID 22240407.
- ^ Štaudová B, Strouhal M, Zobaníková M, Čejková D, Fulton LL, Chen L, Giacani L, Centurion-Lara A, Bruisten SM, Sodergren E, Weinstock GM, Šmajs D (6 November 2014). "Whole Genome Sequence of the Treponema pallidum subsp. endemicum Strain Bosnia A: The Genome Is Related to Yaws Treponemes but Contains Few Loci Similar to Syphilis Treponemes". PLOS Neglected Tropical Diseases. 8 (11): e3261. doi:10.1371/journal.pntd.0003261. ISSN 1935-2735. PMC 4222731. PMID 25375929.
- ^ "Penicillin g benzathine (intramuscular route)". Mayo Clinic. Retrieved 6 November 2024.
- ^ a b Fantry LE, Tramont EC. "Treponema Pallidum (Syphilis)". Infectious Disease and Antimicrobial Agents. Retrieved 12 November 2019 – via www.antimicrobe.org.
- ^ a b c Stamm LV (1 February 2010). "Global Challenge of Antibiotic-Resistant Treponema pallidum". Antimicrobial Agents and Chemotherapy. 54 (2): 583–9. doi:10.1128/AAC.01095-09. PMC 2812177. PMID 19805553.
- ^ Updated recommendations for the treatment of Neisseria gonorrhoeae, Chlamydia trachomatis, and Treponema pallidum (syphilis) and new recommendations on syphilis testing and partner services. World Health Organization. 17 July 2024. doi:10.2471/b09100.
- ^ Lithgow KV, Cameron CE (18 July 2016). "Vaccine development for syphilis". Expert Review of Vaccines. 16 (1): 37–44. doi:10.1080/14760584.2016.1203262. ISSN 1744-8395. PMC 5513191. PMID 27328030.
- ^ Ávila-Nieto C, Pedreño-López N, Mitjà O, Clotet B, Blanco J, Carrillo J (6 April 2023). "Syphilis vaccine: challenges, controversies and opportunities". Frontiers in Immunology. 14. doi:10.3389/fimmu.2023.1126170. ISSN 1664-3224. PMC 10118025. PMID 37090699.
- ^ Bachmann LH (2024). "CDC Clinical Guidelines on the Use of Doxycycline Postexposure Prophylaxis for Bacterial Sexually Transmitted Infection Prevention, United States, 2024". MMWR. Recommendations and Reports. 73 (2): 1–8. doi:10.15585/mmwr.rr7302a1. ISSN 1057-5987. PMC 11166373. PMID 38833414.
- ^ Bishop NH, Miller JN (July 1976). "Humoral immunity in experimental syphilis. I. The demonstration of resistance conferred by passive immunization". Journal of Immunology. 117 (1): 191–6. doi:10.4049/jimmunol.117.1.191. PMID 778261. S2CID 255333392.
- ^ Tomson FL, Conley PG, Norgard MV, Hagman KE (September 2007). "Assessment of cell-surface exposure and vaccinogenic potentials of Treponema pallidum candidate outer membrane proteins". Microbes and Infection. 9 (11): 1267–75. doi:10.1016/j.micinf.2007.05.018. PMC 2112743. PMID 17890130.
- ^ Cameron CE, Lukehart SA (March 2014). "Current status of syphilis vaccine development: need, challenges, prospects". Vaccine. 32 (14): 1602–9. doi:10.1016/j.vaccine.2013.09.053. PMC 3951677. PMID 24135571.
- ^ Penn CW, Bailey MJ, Cockayne A (April 1985). "The axial filament antigen of Treponema pallidum". Immunology. 54 (4): 635–41. PMC 1453562. PMID 3884491.
- ^ Norris SJ (September 1993). "Polypeptides of Treponema pallidum: progress toward understanding their structural, functional, and immunologic roles. Treponema Pallidum Polypeptide Research Group". Microbiological Reviews. 57 (3): 750–79. doi:10.1128/MMBR.57.3.750-779.1993. PMC 372934. PMID 8246847.
- ^ Ávila-Nieto C, Pedreño-López N, Mitjà O, Clotet B, Blanco J, Carrillo J (2023). "Syphilis vaccine: challenges, controversies and opportunities". Frontiers in Immunology. 14: 1126170. doi:10.3389/fimmu.2023.1126170. ISSN 1664-3224. PMC 10118025. PMID 37090699.
Further reading
[edit]- Althouse BM, Hébert-Dufresne L (October 2014). "Epidemic cycles driven by host behaviour". Journal of the Royal Society, Interface. 11 (99): 20140575. doi:10.1098/rsif.2014.0575. PMC 4235258. PMID 25100316.
