User:Vertdegrece/sandbox
| Vertdegrece/sandbox | |
|---|---|
| |
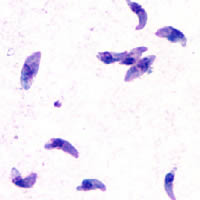
| T. gondii tachyzoites | |
| Scientific classification | |
| Domain: | |
| Kingdom: | |
| Superphylum: | |
| Phylum: | |
| Class: | |
| Subclass: | |
| Order: | |
| Family: | |
| Subfamily: | |
| Genus: | Toxoplasma
|
| Species: | T. gondii
|
| Binomial name | |
| Toxoplasma gondii (Nicolle & Manceaux, 1908)
| |
Toxoplasma gondii (tŏk'sə-plāz'mə gŏn'dē-ī'; T. gondii) is an obligate, intracellular, parasitic protozoan that causes the disease Toxoplasmosis.[1]
Found worldwide, T. gondii is capable of infecting virtually all warm-blooded animals.[2] In humans, it is one of the most common parasites;[3] serological studies estimate that up to a third of the global population has been exposed to and may be chronically infected with T. gondii, although infection rates differ significantly from country to country.[4] Although mild flu-like symptoms occasionally occur during the first few weeks following exposure, infection with T. gondii generally produces no symptoms in healthy, human adults.[5][6] However, in infants, HIV/AIDS patients and others with weakened immunity, infection can cause serious and occasionally fatal illness (see Toxoplasmosis).[5][6]
Infection in humans and other warm-blooded animals can occur:
- by consuming raw or undercooked meat containing T. gondii tissue cysts[7]
- by ingesting water, soil, vegetables, or anything contaminated with oocysts shed in the feces of an infected cat[7]
- through transmission from mother to fetus, particularly when T. gondii is contracted during pregnancy.[7]
Although T. gondii can infect, be transmitted by, and asexually reproduce within humans and virtually all other warm-blooded animals, the parasite can sexually reproduce only within the intestine of members of the cat family (felids).[8] Felids are therefore defined as the definitive hosts of T. gondii, with all other hosts defined as intermediate hosts.
T. gondii has been shown to alter the behavior of infected rodents in ways thought to increase the rodents’ chances of being predated upon by cats.[9][10][11] Because cats are the only hosts within which T. gondii can sexually reproduce to complete and begin its life cycle, such behavioral manipulations are thought to be evolutionary adaptations to increase the parasite’s reproductive success.[11] Although numerous hypotheses exist and are being investigated, the mechanism of T. gondii–induced behavioral changes in rodents remains unknown.[12]
A number of studies have suggested that subtle behavioral or personality changes may occur in infected humans,[13] and infection with parasite has recently been associated with a number of neurological disorders, particularly schizophrenia.[10] However, evidence for causal relationships remain limited.[10]
Life Cycle[edit]

The life cycle of T. gondii can be broadly summarized into two components: 1) a sexual component that occurs only within cats (felids, wild or domestic), and 2) an asexual component that can occur within virtually all warm-blooded animals, including humans, cats, and birds.[14] Because T. gondii can sexually reproduce only within cats, cats are defined as the definitive host of T. gondii. All other hosts – hosts in which only asexual reproduction can occur – are defined as intermediate hosts.
Sexual Reproduction in the Feline Definitive Host[edit]
When a member of the cat family is infected with T. gondii (e.g by consuming an infected mouse laden with T. gondii tissue cysts), the parasite survives passage through the stomach, eventually infecting epithelial cells of the cat’s small intestine.[15] Inside these intestinal cells, T. gondii parasites undergo sexual development and reproduction, producing millions of thick-walled zygote-containing cysts known as oocysts.

Feline Shedding of Oocysts[edit]
Infected epithelial cells eventually rupture and release oocysts into the intestinal lumen, whereupon they are shed in the cat’s feces.[16] Oocysts can then spread to soil, water, food, or anything potentially contaminated with the feces. Highly resilient, oocysts can survive and remain infective for many months in cold and dry climates.[17]
Ingestion of oocysts by humans or other warm-blooded animals is one of the common routes of T. gondii infection.[8] Humans can be exposed to oocysts by, for example, consuming unwashed vegetables or contaminated water, or by handling the feces (litter) of an infected cat.[14][18] Although cats can also be infected by ingesting oocysts, they are much less sensitive to oocyst infection than are intermediate hosts.[19][20]
Inititial Infection of the Intermediate Host[edit]
When an oocyst or tissue cyst is ingested by a human or other warm-blooded animal, the resilient cyst wall is dissolved by proteolytic enzymes in the stomach and small intestine, freeing infectious T. gondii parasites to invade host cells.[8] The parasites first invade cells in and surrounding the intestinal epithelium, and inside these cells, the parasites convert to tachyzoites, the motile and quickly multiplying cellular stage of T. gondii.[15]
Asexual Reproduction in the Intermediate Host[edit]
Inside host cells, T. gondii tachyzoites replicate inside of a specialized vacuole (called the parasitophorous vacuole) created during parasitic entry into the cell.[21] Tachyzoites multiply inside this vacuole until the host cell dies and ruptures, releasing and spreading T. gondii tachyzoites via the blood stream to all organs and tissues of the body, including the brain.[22]

Formation of Tissue Cysts[edit]
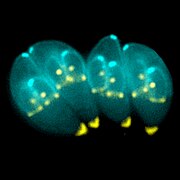
Following the initial period of infection characterized by tachyzoite proliferation throughout the body, pressure from the host’s immune system causes T. gondii tachyzoites to convert into bradyzoites, the semi-dormant, slowly dividing cellular stage of the parasite.[23] Inside host cells, clusters of these slowly dividing bradyzoites are what are known as tissue cysts. The cyst wall is formed by the parasitophorous vacuole membrane.[24] Although bradyzoite-containing tissue cysts can form in virtually any organ, tissue cysts predominantly form and persist in the brain, the eyes, and striated muscle (including the heart).[24] However, specific tissue tropisms can vary between species -- in pigs, the majority of tissue cysts are found in muscle tissue, whereas in mice, the majority of cysts are found in the brain.[25]
Cysts usually range in size between 5-50 µm in diameter,[26] (with 50 µm being about 2/3 the width of the average human hair).[27]
Consumption of tissue cysts in meat is one of the primary means of T. gondii infection, both for humans and for meat-eating warm-blooded animals.[28] Humans consume tissue cysts when eating raw or undercooked meat (particularly pork and lamb).[29] Tissue cyst consumption is the primary means by which cats are infected.[30]
Chronic Infection[edit]
Tissue cysts can be maintained in host tissue for the lifetime of the animal.[31] However, the perpetual presence of cysts appears to be due to a periodic process of cyst rupturing and re-encysting, rather than a perpetual lifespan of individual cysts or bradyzoites.[31] At any given time in a chronically infected host, a very small percentage of cysts are rupturing,[32] although the exact cause of this tissue cysts rupture is, as of 2010, not yet known.[33]
T. gondii can, theoretically, be passed amongst intermediate hosts indefinitely via a cycle of consumption of tissue cysts in meat. However, the parasite’s life cycle begins and completes only when the parasite is passed to a feline host, the only host within which the parasite can again undergo sexual development and reproduction.[8]
Cellular Stages[edit]

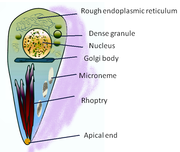
During different periods of T. gondii’s lifecycle, individual parasites convert into various cellular stages, with each stage characterized by a distinct cellular morphology, biochemistry, and behavior. These stages include the tachyzoites, merozoites, bradyzoites (found in tissue cysts), and sporozoites (found in oocysts).
Tachyzoites[edit]
Motile, and quickly multiplying, tachyzoites are responsible for expanding the population of the parasite in the host.[34] When a host consumes a tissue cyst (containing bradyzoites) or an oocyst (containing sporozoites), the bradyzoites or sporozoites stage-convert into tachyzoites upon infecting the intestinal epithelium of the host.[35] During the initial, acute period of infection, tachyzoites spread throughout the body via the blood stream.[22] During the later, latent (chronic) stages of infection, tachyzoites stage-convert to bradyzoites to form tissue cysts.
Merozoites[edit]

Like tachyzoites, merozoites are quickly dividing. Merozites are responsible for expanding the population of the parasite inside the cat intestine prior to sexual reproduction.[34] When a feline definitive host consumes a tissue cyst (containing bradyzoites), bradyzoites convert into merozoites inside intestinal epithelial cells.Following a brief period of rapid population growth in the intestinal epithelium, merozoites convert into the noninfectious sexual stages of the parasite to undergo sexual reproduction, eventually resulting in the formation of zygote (offspring)-containing oocysts.[36]
Bradyzoites[edit]
Bradyzoites are the slowly dividing stage of the parasite that make up tissue cysts. When an uninfected host consumes a tissue cyst, bradyzoites released from the cyst infect intestinal epithelial cells before converting to the proliferative tachyzoite stage.[35] Following the initial period of tachyzoite proliferation throughout the host body, tachyzoites then convert back to bradyzoites, which reproduce inside host cells to form tissue cysts in the new host.
Sporozoites[edit]
Sporozoites are the stage of the parasite residing within oocysts. When a human or other warm-blooded host consumes an oocyst, sporozoites are released from the oocyst, infecting epithelilal cells before converting to the proliferative tachyzoite stage.[35]
Risk Factors for Human Infection[edit]
The following have been identified as being risk factors for T. gondii infection:
- Exposure to or consumption of raw or undercooked meat[37][38][18][39]
- Drinking unpasteurized goat milk[37]
- Contact with soil[7][38]
- Eating unwashed raw vegetables or fruits[18]
- Cleaning cat litter boxes[18]
It should be noted that numerous studies have found that living in a household with a cat is not a significant risk factor for T. gondii infection.[18][38][40]
Preventing Infection[edit]
The following precautions are recommended to prevent or greatly reduce the chances of becoming infected with T. gondii. This information has been adapted from the websites of United States Center for Disease Control and Prevention[41] and the Mayo Clinic.[42]
From food[edit]
- Peel or wash all fruits and vegetables thoroughly before eating.
- Freeze meat for several days at sub-zero temperatures (0° F or -18° C) before cooking. Tissue cysts rarely survive freezing at these temperatures.[43]
- Avoid eating raw or undercooked meat, and never taste meat before fully cooked:
- Cook whole cuts of meat (excluding poultry, see below) to an internal temperature of 145° F (63° C). “Medium rare” meat is generally cooked between 130–140 °F (55–60° C),[44] so cooking whole cuts of meat to “Medium” is recommended. After cooking, a rest period of 3 minutes should be allowed before consumption.
- Cook ground meat (excluding poultry, see below) to an internal temperature of at least 160° F (71° C). This corresponds to having very little to no pink in the center of the meat. No rest time is needed for properly cooked ground meats.
- Cook all poultry (whole or ground) to an internal temperature of at least 165° F (74° C). After cooking, a rest period of 3 minutes should be allowed before consumption.
- Use hot soapy water to wash hands or anything in the kitchen that contacts raw meat, poultry, seafood or unwashed fruits and vegetables.
- Avoid drinking unpasteurized milk.
From environment[edit]
- Change and dispose of cat litter daily. Oocysts in cat feces take at least 1 day to sporulate and become infectious after they are shed, so disposing of cat litter greatly reduces the chances of infectious oocysts being present in litter. Wash hands after changing cat litter.
- Wear gloves when gardening or when in contact with soil or sand, as infectious oocysts from cat feces can spread and survive in the environment for months.
- Avoid drinking untreated water (treated tap water is ok).
- Cover outdoor sandboxes when not being used.
If pregnant or immunocompromised[edit]
- Do not change or handle cat litter boxes. If absolutely necessary, wear gloves and wash hands with hot soapy water immediately afterward.
- Keep cats indoors, and only feed them commercial canned or dry food, or well-cooked table food.
- Do not adopt or handle stray cats, particularly kittens.
- Do not get a new cat while pregnant.
Epidemiology[edit]
In Humans[edit]
T. gondii infections occur throughout the world, although infection rates differ significantly from country to country.[4] For women of childbearing age, a survey of 99 studies within 44 countries found that the areas of highest prevalence are within Latin America (~50-80%), parts of Eastern and Central Europe (~20-60%), the Middle East (~30-50%), parts of Southeast Asia (~20-60%), and parts of Africa (~20-55%).[4]
In the United States, data from the National Health and Nutrition Examination Survey (NHANES) from 1999-2004 found that 9.0% of U.S-born persons 12-49 years of age were seropositive for IgG antibodies against T. gondii, down from 14.1% as measured in the NHANES 1988-1994.[45] In the 1999-2004 survey, 7.7% of U.S-born and 28.1% foreign-born women 15-44 years of age were T. gondii seropositive.[45] A trend of decreasing seroprevalence has been observed by numerous studies both in the United States and in many European countries.[4]
Because the parasite poses a particular threat to fetuses when it is contracted during pregnancy,[46] much of the global epidemiological data regarding T. gondii comes from seropositivity tests in women of childbearing age. Seropositivity tests look for the blood presence of antibodies against T. gondii, so while seropositivity guarantees that one has been exposed to the parasite, it does not necessarily guarantee that one is chronically infected.[47]
In Animals[edit]
Although T. gondii has the capability of infecting virtually all warm-blooded animals, susceptibility and rates of infection vary widely between different genera and species.[48] Rates of infection in populations of the same species can also vary widely due to differences in location, diet, and other factors.
Livestock[edit]
Among livestock, pigs, sheep, and goats have the highest rates of chronic T. gondii infection.[7] The prevalence of T. gondii in meat-producing animals varies widely both within and between countries,[7] and rates of infection have been shown to be dramatically influenced by varying farming and management practices.[49] For instance, animals kept outdoors or in free-ranging environments are more at risk of T. gondii infection than animals raised indoors or in commercial confinement operations.[29][49]
In the United States, the percentage of pigs harboring viable parasite has been measured (via bioassay in mice or cats) to be as high as 92.7% and as low as 0%, depending on the farm or herd.[29] Surveys of seroprevalence (T. gondii antibodies in blood) are more common, and such measurements are indicative of the high relative seroprevlance in pigs across the world.[50] Along with pigs, sheep and goats are among the most commonly infected livestock of epidemiological significance for human infection.[7] Prevalence of viable T. gondii in sheep tissue has been measured (via bioassay) to be as high as 78% in the United States,[51] and a 2011 survey of goats intended for consumption in the United States found a seroprevalence of 53.4%.[52]
Due to a lack of exposure to the outdoors, chickens raised in large-scale indoor confinement operations are not commonly infected with T. gondii.[49] Free-ranging or backyard-raised chickens are much more commonly infected.[49] A survey of free-ranging chickens in the United States found T. gondii prevalence to be 17%-100%, depending on the farm.[53] Because chicken meat is generally cooked thoroughly before consumption, poultry is not generally considered to be a significant risk factor for human T. gondii infection.[54]
Although cattle and buffalo can be infected with T. gondii, the parasite is generally eliminated or reduced to undetectable levels within a few weeks following exposure.[49] Tissue cysts are rarely present in buffalo or cattle beef, and meat from these animals is considered to be at low-risk for harboring viable parasite.[7][29]
Horses are considered resistant to chronic T. gondii infection.[49] However, viable T. gondii has been isolated from United States horses slaughtered for export, and severe human toxoplasmosis in France has been epidemiologically linked to the consumption of horse meat.[29]
Domestic Cats[edit]
The seroprevalence of T. gondii in domestic cats, worldwide, has been estimated to be around 30-40%.[55] In the United States, there has been no official national estimate, but local surveys have varied between ~16% to 80%.[55] A 2012 survey of 445 purebred pet cats and 45 shelter cats in Finland found an overall seroprevalence of 48.4%.[56] A 2010 survey of feral cats from Giza, Egypt found an overall seroprevalence of 97.4%.[57]
The infection rate of domestic cats varies widely depending on cats’ lifestyle.[58] Feral cats that hunt for their food are more likely to be infected than domestic cats. The prevalence of T. gondii in cat populations depends on the availability of infected birds and small mammals,[30] but often this availability is abundant. In the United States alone, free-ranging domestic cats are estimated to kill 1.4-3.7 billion birds and 6.9-20.7 billion mammals each year.[59]
Most infected cats will shed oocysts only once in their lifetime, for a period of about one to two weeks.[55] Although this period of shedding is quite transient, millions of oocysts can be shed during this time, with each oocyst capable of spreading and surviving for months.[55] It has been estimated that about 1% of cats at any given time are actively shedding oocysts.[49]
Behavioral Changes in Rodents[edit]
Infection with T. gondii has been shown to alter the behavior of mice and rats in ways thought to increase the rodents’ chances of being predated upon by cats.[9][60][11] Infected rodents show a reduction in their innate aversion to cat odors; while uninfected mice and rats will generally avoid areas marked with cat urine or with cat body odor, this avoidance is reduced or eliminated in infected animals.[60][11][61] Moreover, there is some evidence to suggest that this loss-of-aversion may be specific to feline odors: when given a choice between two predator odors (cat or mink), infected rodents show a significantly stronger preference to cat odors than do uninfected controls.[62][63]
T. gondii infected rodents show a number of behavioral changes beyond altered responses to cat odors. Rats infected with the parasite show increased levels of activity and decreased neophobic behavior.[9][12] Similarly, infected mice show alterations in patterns of locomotion and exploratory behavior during experimental tests. These patterns include traveling further distances, moving at higher speeds, accelerating for longer periods of time, and showing a decreased pause-time when placed in new arenas.[64] Infected rodents have also been shown to have differences in traditional measures of anxiety such as elevated plus mazes, open field arenas, and social interaction tests.[64][65]
Despite being seropositive for anti-T.gondii antibodies, not all rodents that are naturally or experimentally exposed to the parasite become chronically infected and develop tissue cysts in the brain.[47][64] There is accumulating evidence that behavioral changes in experimentally exposed rodents only occur in the subset of animals with brain tissue cysts (that is, animals confirmed to be chronically infected).[64]
The mechanisms by which T. gondii alters host behavior remain unknown.[12]
Physiological and Behavioral Changes in Humans[edit]
Chronic infection with T. gondii has traditionally been considered asymptomatic in immunocompetent human hosts. However, there is accumulating evidence suggesting that latent infection may subtly influence a range of human behaviors and tendencies, and that infection may alter the susceptibility to or intensity of a number of affective, psychiatric, or neurological disorders.[10]
Latent T. gondii infection in humans has been associated with impaired psychomotor performance, enhanced risk-taking personality profiles, and higher incidents of automobile accidents.[10] Moreover, correlations have been found between positive antibody titers to T. gondii and OCD, Parkinson’s disease, Alzheimer’s disease, suicide in patients with mood disorders, and bipolar disorder.[10] Positive antibody titers to T. gondii have been shown to be not correlative with major depression or dysthymia.[66]
The most substantial body of evidence linking T. gondii to a neurological disorder involves the potential association between schizophrenia and infection with the parasite.[67][60] As of 2013, at least 38 studies have found a positive correlation between T. gondii antibody titers and schizophrenia.[10][68] While the vast majority of these studies tested patients already diagnosed with schizophrenia for T. gondii antibodies, significant associations between T. gondii and schizophrenia have been found prior to the onset of schizophrenia disease symptoms.[60]
Limitations[edit]
In most of the current studies where positive associations have been found between T. gondii antibody titers and certain behavioral traits or neurological disorders, it is important to note that T. gondii seropositivity tests are conducted after the onset of the examined disease or behavioral trait; that is, it is often unclear whether infection with the parasite increases the the chances of having a certain trait or disorder, or if having a certain trait or disorder increases the chances of becoming infected with the parasite.[13] It has been suggested that groups of individuals with certain behavioral traits or neurological disorders may share certain behavioral tendencies that increase the likelihood of exposure to and infection by T. gondii.[13]
History[edit]
In 1908, while working at the Pasteur Institute in Tunis, Charles Nicolle and Louis Manceaux discovered a protozoan organism in the tissues of a hamster-like rodent known as the gundi, Ctenodactylus gundi.[8] Although Nicolle and Mancaeux initially believed the organism to be the parasite Leishmania, they soon realized that they had discovered a new organism entirely. They named it Toxoplasma gondii, a reference to it's morphology (Toxo, modified from the latin prefix tox-/toxi-/toxo- meaning arc-like or bow-like + plasma, latin for image) and the host in which it was discovered, the gundi (gondii). The same year that Nicolle and Mancaeux discovered T. gondii, Alfonso Splendore identified the same organism in a rabbit in Brazil. However, he did not give it a name it.[8]
The first conclusive identification of T. gondii in humans was in an infant girl delivered full term by Caesarean section on May 23, 1938 at Babies Hospital in New York.[8] The girl began having seizures at 3 days of age, and doctors identified lesions in the maculae of both of her eyes. When she died at 1 month of age, an autopsy was performed. Lesions discovered in her brain and eye tissue were found to have both free and intracellular T. gondii.[8] Infected tissue from the girl was homogenized and inoculated intracerebrally into rabbits and mice; the animals subsequently developed encephalitis. Later, congenital transmission was found to occur in numerous other species, particularly in sheep and in rodents.
The possibility of T. gondii transmission via consumption of undercooked meat was first proposed by D. Weinman and A.H Chandler in 1954.[8] In 1960, it was shown that the cyst wall of tissue cysts immediately dissolved in proteolytic enzymes found in the stomach, but that the released T. gondii bradyzoites could survive long enough to infect the host. The hypothesis of transmission via undercooked meat was tested in an orphanage in Paris in 1965; yearly acquisition rates of T. gondii rose from 10% to 50% after adding two portions of barely cooked beef or horse meat to the orphans' daily diet, and to 100% after adding barely cooked lamb chops.[8]
In 1959, a study in Bombay found the prevalence of T. gondii in strict vegetarians to be similar to that found in non-vegetarians. This raised the possibility of a third major route of infection, beyond congenital and carnivorous transmission. [8] In 1970, the existence of T. gondii oocysts was discovered in cat feces, and the fecal-oral route of infection via oocysts was demonstrated.[8]
Throughout the 1970s and 1980s, a vast number of species were tested for the ability to shed oocysts upon infection. Whereas at least 17 different species of felids have been confirmed to shed oocysts, no non-felid has been shown to be permissive for T. gondii sexual reproduction and subsequent oocyst shedding.[8]
References[edit]
- ^ Louis M Weiss, Kami Kim (2011) p. 49
- ^ J.P Dubey (2010) p. 1
- ^ "CDC - About Parasites". Retrieved 12 March 2013.
- ^ a b c d Pappas, G.; Roussos, N.; Falagas, M. E. (2009 Oct). "Toxoplasmosis snapshots: global status of Toxoplasma gondii seroprevalence and implications for pregnancy and congenital toxoplasmosis". International Journal for Parasitology. 39 (12): 1385–94. doi:10.1016/j.ijpara.2009.04.003. PMID 19433092.
{{cite journal}}: Check date values in:|date=(help) - ^ a b "CDC Parasites - Toxoplasmosis (Toxoplasma infection) - Disease". Retrieved 12 March 2013.
- ^ a b J.P Dubey (2010) p. 77
- ^ a b c d e f g h Tenter, A. M.; Heckeroth, A. R.; Weiss, L. M. (2000 Nov). "Toxoplasma gondii: from animals to humans". International Journal for Parasitology. 30 (12–13): 1217–58. doi:10.1016/s0020-7519(00)00124-7. PMC 3109627. PMID 11113252.
{{cite journal}}: Check date values in:|date=(help) - ^ a b c d e f g h i j k l m Dubey, JP (2009 Jul 1). "History of the discovery of the life cycle of Toxoplasma gondii". International Journal for Parasitology. 39 (8): 877–82. doi:10.1016/j.ijpara.2009.01.005. PMID 19630138.
{{cite journal}}: Check date values in:|date=(help) - ^ a b c Webster, JP (2007 May). "The effect of Toxoplasma gondii on animal behavior: playing cat and mouse". Schizophrenia Bulletin. 33 (3): 752–6. doi:10.1093/schbul/sbl073. PMC 2526137. PMID 17218613.
{{cite journal}}: Check date values in:|date=(help) - ^ a b c d e f g Webster, J. P.; Kaushik, M.; Bristow, G. C.; McConkey, G. A. (2013 Jan 1). "Toxoplasma gondii infection, from predation to schizophrenia: can animal behaviour help us understand human behaviour?". The Journal of Experimental Biology. 216 (Pt 1): 99–112. doi:10.1242/jeb.074716. PMC 3515034. PMID 23225872.
{{cite journal}}: Check date values in:|date=(help) - ^ a b c d Berdoy, M.; Webster, J. P.; MacDonald, D. W. (2000 Aug 7). "Fatal attraction in rats infected with Toxoplasma gondii". Proceedings. Biological Sciences / The Royal Society. 267 (1452): 1591–4. doi:10.1098/rspb.2000.1182. PMC 1690701. PMID 11007336.
{{cite journal}}: Check date values in:|date=(help) - ^ a b c McConkey, G. A.; Martin, H. L.; Bristow, G. C.; Webster, J. P. (2013 Jan 1). "Toxoplasma gondii infection and behaviour - location, location, location?". The Journal of Experimental Biology. 216 (Pt 1): 113–9. doi:10.1242/jeb.074153. PMC 3515035. PMID 23225873.
{{cite journal}}: Check date values in:|date=(help) - ^ a b c Flegr, J (2013 Jan 1). "Influence of latent Toxoplasma infection on human personality, physiology and morphology: pros and cons of the Toxoplasma-human model in studying the manipulation hypothesis". The Journal of Experimental Biology. 216 (Pt 1): 127–33. doi:10.1242/jeb.073635. PMID 23225875.
{{cite journal}}: Check date values in:|date=(help) - ^ a b Louis M Weiss, Kami Kim (2011) p. 2
- ^ a b Louis M Weiss, Kami Kim (2011) p. 39
- ^ J.P Dubey (2010) p. 22
- ^ Dubey, J. P.; Ferreira, L. R.; Martins, J.; Jones, J. L. (2011 Oct). "Sporulation and survival of Toxoplasma gondii oocysts in different types of commercial cat litter". The Journal of Parasitology. 97 (5): 751–4. doi:10.1645/GE-2774.1. PMID 21539466.
{{cite journal}}: Check date values in:|date=(help) - ^ a b c d e Kapperud, G.; Jenum, P. A.; Stray-Pedersen, B.; Melby, K. K.; Eskild, A.; Eng, J. (1996 Aug 15). "Risk factors for Toxoplasma gondii infection in pregnancy. Results of a prospective case-control study in Norway". American Journal of Epidemiology. 144 (4): 405–12. doi:10.1093/oxfordjournals.aje.a008942. PMID 8712198.
{{cite journal}}: Check date values in:|date=(help) - ^ Dubey, JP (1998 Jul). "Advances in the life cycle of Toxoplasma gondii". International Journal for Parasitology. 28 (7): 1019–24. doi:10.1016/s0020-7519(98)00023-x. PMID 9724872.
{{cite journal}}: Check date values in:|date=(help) - ^ J.P Dubey (2010) p. 107
- ^ Louis M Weiss, Kami Kim (2011) p. 23-29
- ^ a b Louis M Weiss, Kami Kim (2011) p. 39-40
- ^ Miller, C. M.; Boulter, N. R.; Ikin, R. J.; Smith, N. C. (2009 Jan). "The immunobiology of the innate response to Toxoplasma gondii". International Journal for Parasitology. 39 (1): 23–39. doi:10.1016/j.ijpara.2008.08.002. PMID 18775432.
{{cite journal}}: Check date values in:|date=(help) - ^ a b Louis M Weiss, Kami Kim (2011) p. 343
- ^ Louis M Weiss, Kami Kim (2011) p. 41
- ^ "CDC Toxoplasmosis - Microscopy Findings". Retrieved 13 March 2013.
- ^ Clarence R. Robbins (24 February 2012). Chemical and Physical Behavior of Human Hair. Springer. p. 585. ISBN 978-3-642-25610-3. Retrieved 12 March 2013.
- ^ Louis M Weiss, Kami Kim (2011) p. 3
- ^ a b c d e Jones, J. L.; Dubey, J. P. (2012 Sep). "Foodborne toxoplasmosis". Clinical Infectious Diseases : An Official Publication of the Infectious Diseases Society of America. 55 (6): 845–51. doi:10.1093/cid/cis508. PMID 22618566.
{{cite journal}}: Check date values in:|date=(help) - ^ a b J.P Dubey (2010) p. 46
- ^ a b Louis M Weiss, Kami Kim (2011) p. 580
- ^ Louis M Weiss, Kami Kim (2011) p. 45
- ^ J.P Dubey (2010) p. 47
- ^ a b Louis M Weiss, Kami Kim (2011) p. 19
- ^ a b c Louis M Weiss, Kami Kim (2011) p. 359
- ^ Louis M Weiss, Kami Kim (2011) p. 306
- ^ a b Jones, J. L.; Dargelas, V.; Roberts, J.; Press, C.; Remington, J. S.; Montoya, J. G. (2009 Sep 15). "Risk factors for Toxoplasma gondii infection in the United States". Clinical Infectious Diseases : An Official Publication of the Infectious Diseases Society of America. 49 (6): 878–84. doi:10.1086/605433. PMID 19663709.
{{cite journal}}: Check date values in:|date=(help) - ^ a b c Cook, A. J.; Gilbert, R. E.; Buffolano, W.; Zufferey, J.; Petersen, E.; Jenum, P. A.; Foulon, W.; Semprini, A. E.; Dunn, D. T. (2000 Jul 15). "Sources of toxoplasma infection in pregnant women: European multicentre case-control study. European Research Network on Congenital Toxoplasmosis". BMJ (Clinical Research Ed.). 321 (7254): 142–7. doi:10.1136/bmj.321.7254.142. PMC 27431. PMID 10894691.
{{cite journal}}: Check date values in:|date=(help) - ^ Sakikawa, M.; Noda, S.; Hanaoka, M.; Nakayama, H.; Hojo, S.; Kakinoki, S.; Nakata, M.; Yasuda, T.; Ikenoue, T.; Kojima, T. (2012 Mar). "Anti-Toxoplasma antibody prevalence, primary infection rate, and risk factors in a study of toxoplasmosis in 4,466 pregnant women in Japan". Clinical and Vaccine Immunology : CVI. 19 (3): 365–7. doi:10.1128/CVI.05486-11. PMC 3294603. PMID 22205659.
{{cite journal}}: Check date values in:|date=(help) - ^ Bobić, B.; Jevremović, I.; Marinković, J.; Sibalić, D.; Djurković-Djaković, O. (1998 Sep). "Risk factors for Toxoplasma infection in a reproductive age female population in the area of Belgrade, Yugoslavia". European Journal of Epidemiology. 14 (6): 605–10. doi:10.1023/a:1007461225944. PMID 9794128.
{{cite journal}}: Check date values in:|date=(help) - ^ "CDC: Parasites - Toxoplasmosis (Toxoplasma infection) - Prevention & Control". Retrieved 13 March 2013.
- ^ "Mayo Clinic - Toxoplasmosis - Prevention". Retrieved 13 March 2013.
- ^ J.P Dubey (2010) p. 45
- ^ Green, Aliza (2005). Field Guide to Meat. Philadelphia, PA: Quirk Books. pp. 294–295. ISBN 1594740178.
- ^ a b Jones, J. L.; Kruszon-Moran, D.; Sanders-Lewis, K.; Wilson, M. (2007 Sep). "Toxoplasma gondii infection in the United States, 1999 2004, decline from the prior decade". The American Journal of Tropical Medicine and Hygiene. 77 (3): 405–10. doi:10.4269/ajtmh.2007.77.405. PMID 17827351.
{{cite journal}}: Check date values in:|date=(help) - ^ "CDC: Parasites - Toxoplasmosis (Toxoplasma infection) - Pregnant Women". Retrieved 13 March 2013.
- ^ a b Dubey, J. P.; Frenkel, J. K. (1998 May). "Toxoplasmosis of rats: a review, with considerations of their value as an animal model and their possible role in epidemiology". Veterinary Parasitology. 77 (1): 1–32. doi:10.1016/s0304-4017(97)00227-6. PMID 9652380.
{{cite journal}}: Check date values in:|date=(help) - ^ J.P Dubey (2010)
- ^ a b c d e f g Dubey, J. P.; Jones, J. L. (2008 Sep). "Toxoplasma gondii infection in humans and animals in the United States". International Journal for Parasitology. 38 (11): 1257–78. doi:10.1016/j.ijpara.2008.03.007. PMID 18508057.
{{cite journal}}: Check date values in:|date=(help) - ^ J.P Dubey (2010) p. 145-151
- ^ Dubey, J. P.; Sundar, N.; Hill, D.; Velmurugan, G. V.; Bandini, L. A.; Kwok, O. C.; Majumdar, D.; Su, C. (2008 Jul). "High prevalence and abundant atypical genotypes of Toxoplasma gondii isolated from lambs destined for human consumption in the USA". International Journal for Parasitology. 38 (8–9): 999–1006. doi:10.1016/j.ijpara.2007.11.012. PMID 18191859.
{{cite journal}}: Check date values in:|date=(help) - ^ Dubey, J. P.; Rajendran, C.; Ferreira, L. R.; Martins, J.; Kwok, O. C.; Hill, D. E.; Villena, I.; Zhou, H.; Su, C.; Jones, J. L. (2011 Jul). "High prevalence and genotypes of Toxoplasma gondii isolated from goats, from a retail meat store, destined for human consumption in the USA". International Journal for Parasitology. 41 (8): 827–33. doi:10.1016/j.ijpara.2011.03.006. PMID 21515278.
{{cite journal}}: Check date values in:|date=(help) - ^ Dubey, JP (2010 Feb). "Toxoplasma gondii infections in chickens (Gallus domesticus): prevalence, clinical disease, diagnosis and public health significance". Zoonoses and Public Health. 57 (1): 60–73. doi:10.1111/j.1863-2378.2009.01274.x. PMID 19744305.
{{cite journal}}: Check date values in:|date=(help) - ^ Louis M Weiss, Kami Kim (2011) p. 723
- ^ a b c d Elmore, S. A.; Jones, J. L.; Conrad, P. A.; Patton, S.; Lindsay, D. S.; Dubey, J. P. (2010 Apr). "Toxoplasma gondii: epidemiology, feline clinical aspects, and prevention". Trends in Parasitology. 26 (4): 190–6. doi:10.1016/j.pt.2010.01.009. PMID 20202907.
{{cite journal}}: Check date values in:|date=(help) - ^ Jokelainen, P.; Simola, O.; Rantanen, E.; Näreaho, A.; Lohi, H.; Sukura, A. (2012 Nov). "Feline toxoplasmosis in Finland: cross-sectional epidemiological study and case series study". Journal of Veterinary Diagnostic Investigation : Official Publication of the American Association of Veterinary Laboratory Diagnosticians, Inc. 24 (6): 1115–24. doi:10.1177/1040638712461787. PMID 23012380.
{{cite journal}}: Check date values in:|date=(help) - ^ Al-Kappany, Y. M.; Rajendran, C.; Ferreira, L. R.; Kwok, O. C.; Abu-Elwafa, S. A.; Hilali, M.; Dubey, J. P. (2010 Dec). "High prevalence of toxoplasmosis in cats from Egypt: isolation of viable Toxoplasma gondii, tissue distribution, and isolate designation". The Journal of Parasitology. 96 (6): 1115–8. doi:10.1645/GE-2554.1. PMID 21158619.
{{cite journal}}: Check date values in:|date=(help) - ^ J.P Dubey (2010) p. 95
- ^ Loss, S. R.; Will, T.; Marra, P. P. (2013 Jan 29). "The impact of free-ranging domestic cats on wildlife of the United States". Nature Communications. 4: 1396. doi:10.1038/ncomms2380. PMID 23360987.
{{cite journal}}: Check date values in:|date=(help) - ^ a b c d Webster, J. P.; McConkey, G. A. (2010 Jun). "Toxoplasma gondii-altered host behaviour: clues as to mechanism of action". Folia Parasitologica. 57 (2): 95–104. doi:10.14411/fp.2010.012. PMID 20608471.
{{cite journal}}: Check date values in:|date=(help) - ^ Vyas, A.; Kim, S. K.; Giacomini, N.; Boothroyd, J. C.; Sapolsky, R. M. (2007 Apr 10). "Behavioral changes induced by Toxoplasma infection of rodents are highly specific to aversion of cat odors". Proceedings of the National Academy of Sciences of the United States of America. 104 (15): 6442–7. doi:10.1073/pnas.0608310104. PMC 1851063. PMID 17404235.
{{cite journal}}: Check date values in:|date=(help) - ^ Xiao, J.; Kannan, G.; Jones-Brando, L.; Brannock, C.; Krasnova, I. N.; Cadet, J. L.; Pletnikov, M.; Yolken, R. H. (2012 Mar 29). "Sex-specific changes in gene expression and behavior induced by chronic Toxoplasma infection in mice". Neuroscience. 206: 39–48. doi:10.1016/j.neuroscience.2011.12.051. PMID 22240252.
{{cite journal}}: Check date values in:|date=(help) - ^ Lamberton, PH (2008 Sep). "Specificity of the Toxoplasma gondii-altered behaviour to definitive versus non-definitive host predation risk". Parasitology. 135 (10): 1143–50. doi:10.1017/S0031182008004666. PMID 18620624.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ a b c d Afonso, C.; Paixão, V. B.; Costa, R. M. (2012). "Chronic Toxoplasma infection modifies the structure and the risk of host behavior". PLOS ONE. 7 (3): e32489. doi:10.1371/journal.pone.0032489. PMC 3303785. PMID 22431975.
- ^ Gonzalez, L. E.; Rojnik, B.; Urrea, F.; Urdaneta, H.; Petrosino, P.; Colasante, C.; Pino, S.; Hernandez, L. (2007 Feb 12). "Toxoplasma gondii infection lower anxiety as measured in the plus-maze and social interaction tests in rats A behavioral analysis". Behavioural Brain Research. 177 (1): 70–9. doi:10.1016/j.bbr.2006.11.012. PMID 17169442.
{{cite journal}}: Check date values in:|date=(help) - ^ Pearce, B. D.; Kruszon-Moran, D.; Jones, J. L. (2012 Aug 15). "The relationship between Toxoplasma gondii infection and mood disorders in the third National Health and Nutrition Survey". Biological Psychiatry. 72 (4): 290–5. doi:10.1016/j.biopsych.2012.01.003. PMC 4750371. PMID 22325983.
{{cite journal}}: Check date values in:|date=(help) - ^ Torrey, E. F.; Yolken, R. H. (2007 May). "Schizophrenia and toxoplasmosis". Schizophrenia Bulletin. 33 (3): 727–8. doi:10.1093/schbul/sbm026. PMC 2526129. PMID 17426051.
{{cite journal}}: Check date values in:|date=(help) - ^ Torrey, E. F.; Bartko, J. J.; Yolken, R. H. (2012 May). "Toxoplasma gondii and other risk factors for schizophrenia: an update". Schizophrenia Bulletin. 38 (3): 642–7. doi:10.1093/schbul/sbs043. PMC 3329973. PMID 22446566.
{{cite journal}}: Check date values in:|date=(help)
Bibliography[edit]
- Louis M Weiss; Kami Kim (28 April 2011). Toxoplasma Gondii: The Model Apicomplexan. Perspectives and Methods. Academic Press. ISBN 978-0-08-047501-1. Retrieved 12 March 2013.
- J. P. Dubey (15 April 2010). Toxoplasmosis of Animals and Humans, Second Edition. CRC Press. ISBN 978-1-4200-9237-0. Retrieved 12 March 2013.
External links[edit]
- ToxoDB : The Toxoplasma gondii genome resource
- Anti-Toxo : A Toxoplasma news blog and list of research laboratories
- Toxoplasma images, from CDC's DPDx, in the public domain
- Toxoplasmosis Research Institute & Center
- Cytoskeletal Components of an Invasion Machine — The Apical Complex of Toxoplasma gondii
- The Culture-Shaping Parasites, in Seed Magazine
- Sneaky Parasite Attracts Rats to Cats, All Things Considered, April 14, 2007
- Toxoplasma overview, developmental stages, life cycle image at MetaPathogen
- Toxoplasma lecture, Robert Sapolsky
- [dead link] Could a brain parasite found in cats help soccer teams win at the World Cup? - By Patrick House - Slate Magazine
- How Your Cat Is Making You Crazy, the Atlantic Magazine, March 2012
- Mystery Marine Mammal Deaths, CosmosMagazine.com, June 2008
- Toxoplasma gondii in the Subarctic and Arctic
- The T.Gondii host/pathogen interactome
- Toxoplasmosis - Recent advances, Open access book published in September 2012
- Toxoplasma gondii, the Immune System, and Suicidal Behaviour
Category:Apicomplexa
Category:Protists described in 1908
Category:Suicide-inducing parasitism
Category:Cat diseases

