Rose bengal
| |
| Names | |
|---|---|
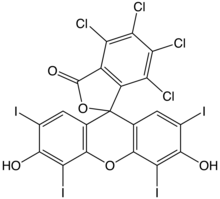
| Preferred IUPAC name
4,5,6,7-Tetrachloro-3′,6′-dihydroxy-2′,4′,5′,7′-tetraiodo-3H-spiro[[2]benzofuran-1,9′-xanthen]-3-one | |
| Other names
* C.I. 45440
| |
| Identifiers | |
3D model (JSmol)
|
|
| ChEMBL | |
| ChemSpider | |
| ECHA InfoCard | 100.021.813 |
| EC Number |
|
PubChem CID
|
|
| UNII | |
CompTox Dashboard (EPA)
|
|
| |
| |
| Properties | |
| C20H4Cl4I4O5 | |
| Molar mass | 973.67 g/mol 1,017.65 g/mol (sodium salt) |
| Pharmacology | |
| S01JA02 (WHO) | |
| Hazards | |
| GHS labelling: | |

| |
| Warning | |
| H315, H319, H335 | |
| P261, P264, P271, P280, P302+P352, P304+P340, P305+P351+P338, P312, P321, P332+P313, P337+P313, P362, P403+P233, P405, P501 | |
Except where otherwise noted, data are given for materials in their standard state (at 25 °C [77 °F], 100 kPa).
| |

Rose bengal (4,5,6,7-tetrachloro-2',4',5',7'-tetraiodofluorescein) is a stain. Rose bengal belongs to the class of organic compounds called xanthenes.[1] Its sodium salt is commonly used in eye drops to stain damaged conjunctival and corneal cells and thereby identify damage to the eye. The stain is also used in the preparation of Foraminifera for microscopic analysis, allowing the distinction between forms that were alive or dead at the time of collection.
A form of rose bengal is also being studied as a treatment for certain cancers and skin conditions. The cancer formulation of the drug, known as PV-10, is currently undergoing clinical trials for melanoma,[2] breast cancer.[3] and neuroendocrine tumors. The company also has formulated a drug based on rose bengal for the treatment of eczema and psoriasis; this drug, PV-10, is currently in clinical trials as well.[2]
History and etymology
[edit]Rose bengal was originally prepared in 1882 by Swiss chemist Robert Ghnem, as an analogue of fluorescein.[4] Rudolf Nietzki at the University of Basel identified the principal constituents of rose bengal as iodine derivatives of di- and tetra-chlorofluorescein.[5] The compound was originally used as a wool dye.[6] Its name derives from rose (flower) and Bengal (region); it is printed as rose bengal or Rose Bengal in the scientific literature.[7]
Chemical applications
[edit]
Despite its complicated photochemistry involving several species,[8] rose bengal is also used in synthetic chemistry as a visible light photoredox catalyst[9] and to generate singlet oxygen from triplet oxygen. The singlet oxygen can then undergo a variety of useful reactions, particularly [2 + 2] cycloadditions with alkenes and similar systems.
Derivatives and salts
[edit]Rose bengal can be used to form many derivatives that have important medical functions. One such derivative was created so to be sonosensitive but photoinsensitive, so that with a high intensity focused ultrasound, it could be used in the treatment of cancer. The derivative was formed by amidation of rose bengal, which turned off the fluorescent and photosensitive properties of rose bengal, leading to a usable compound, named in the study as RB2.[10]

Salts of rose bengal include C20H2Cl4I4Na2O5 (CAS 632-69-9). This sodium salt is a dye, which has its own unique properties and uses.[11]
Biological applications
[edit]

PV-10 (an injectable form of rose bengal) was found to cause an observable response in 60% of tumors treated, according to researchers in a phase II melanoma study. Locoregional disease control was observed in 75% of patients. Also confirmed was a "bystander effect", previously observed in the phase I trial, whereby untreated lesions responded to treatment as well, potentially due to immune system response. These data were based on the interim results (in 2009) of the first 40 patients treated in an 80-patient study.[3][needs update] As of April 2016[update] a phase-3 study of PV-10 as a single agent therapy for patients with locally advanced cutaneous melanoma (Clinical Trials ID NCT02288897) is enrolling patients.[2]
Rose bengal has been shown to not just prevent the growth and spread of ovarian cancer, but also to cause apoptotic cell death of the cancer cells. This has been proven in vitro, in order to prove that rose bengal is still a possible option in the treatment of cancer, and further research should be done.[12]
Rose bengal has been used to treat colon cancer. In one such study,[13] a protective immune response was generated from immunogenic cell death.
Rose bengal is also used in animal models of ischemic stroke (photothrombotic stroke models) in biomedical research. A bolus of the compound is injected into the venous system. Then the region of interest (e.g., the cerebral cortex) is exposed and illuminated by LASER light of 561 nm. A thrombus is formed in the illuminated blood vessels, causing a stroke in the dependent brain tissue.[14][15]
Rose bengal has been used for 50 years to diagnose liver and eye cancer. Rose bengal dye is mixed with the homogenate of Brucella and pH of the solution is maintained at 3.8, and this dye is used to diagnose Brucellosis by agglutinating the suspected serum. Rose bengal is slightly irritating and toxic to the eye.[6] It has also been used as an insecticide.[16][17]
Rose bengal is able to stain cells whenever the surface epithelium is not being properly protected by the preocular tear film, because rose bengal has been proven to not be able to stain cells because of the protective functioning of these preocular tear films.[18] This is why rose bengal is often useful as a stain in diagnosing certain medical issues, such as conjunctival and lid disorders.[19]
Rose bengal has been used for ocular surface staining to study the efficacy of punctal plugs in the treatment of keratoconjunctivitis sicca.[20]
Rose bengal is being researched as an agent in creating nano sutures.[21] Wounds are painted on both sides with it and then illuminated with an intense light. This links the tiny collagen fibers together sealing the wound.[22][23][24] Healing is faster and the seal reduces chances of infection.[25][26]
Rose bengal is used to suppress bacterial growth in several microbiological media, including Cooke's rose bengal agar.
Rose bengal has been used as a protoplasm stain to discriminate between living and dead micro-organisms, particularly Foraminifera, since the 1950s when Bill Walton developed the technique.[27]
Rose bengal acetate can act as a photosensitiser and may have potential in photodynamic therapy to treat some cancers.[28]
References
[edit]- ^ "Rose Bengal Compound Summary". PubChem.
- ^ a b c Provectus Biopharmaceuticals Reports Data On PV-10 in Combination Therapy and T Cell Mediated Immunity Presented at American Association for Cancer Research (AACR) Annual Meeting 2016. April 2016
- ^ a b Metastatic Melanoma PV-10 Trial Results Encouraging Says Drug Company, Medical News Today, 9 June 2009
- ^ Alexander W (2010). "American Society of Clinical Oncology, 2010 Annual Meeting and Rose Bengal: From a Wool Dye to a Cancer Therapy". Pharmacy and Therapeutics. 35 (8): 469–474. PMC 2935646. PMID 20844697.
- ^ Orellana C. "Rose Bengal The pink eye stain that might be a cancer treatment".
- ^ a b Orellana C. "Rose Bengal--the Pink Eye Stain that might be a Cancer Treatment".
- ^ Senning, Alexander (2006). Elsevier's Dictionary of Chemoetymology: The Whys and Whences of Chemical Nomenclature and Terminology. Elsevier. p. 344. ISBN 978-0-08-048881-3.
- ^ Ludvíková L, Friš P, Heger D, Šebej P, Wirz J, Klán P (2016). "Photochemistry of rose bengal in water and acetonitrile: a comprehensive kinetic analysis". Physical Chemistry Chemical Physics. 18 (24): 16266–16273. Bibcode:2016PCCP...1816266L. doi:10.1039/C6CP01710J. ISSN 1463-9076. PMID 27253480.
- ^ Romero NA, Nicewicz DA (2016-09-14). "Organic Photoredox Catalysis". Chemical Reviews. 116 (17): 10075–10166. doi:10.1021/acs.chemrev.6b00057. ISSN 0009-2665. PMID 27285582.
- ^ Kim Y, Valentina Rubio, Jianjun Qi, Rongmin Xia, Zheng-Zheng Shi, Leif Peterson, Ching-Hsuan Tung, Brian E. O'Neill (2012). "Cancer treatment using an optically inert rose bengal derivative combined with pulsed focused ultrasound". AIP Conference Proceedings. 1481 (1): 175. Bibcode:2012AIPC.1481..175K. doi:10.1063/1.4757330. Published as Kim YS, Rubio V, Qi J, Xia R, Shi ZZ, Peterson L, Tung CH, O'Neill BE (2011). "Cancer treatment using an optically inert Rose Bengal derivative combined with pulsed focused ultrasound". J Control Release. 156 (3): 315–22. doi:10.1016/j.jconrel.2011.08.016. PMC 3230682. PMID 21871506.
- ^ "Rose Bengal Sodium Salt". Sigma-Aldrich. Sigma Aldrich Co. Retrieved 12 November 2013.
- ^ Koevary S (2012). "Selective toxicity of rose bengal to ovarian cancer cells in vitro". International Journal of Physiology, Pathophysiology and Pharmacology. 4 (2): 99–107. PMC 3403562. PMID 22837809.
- ^ Qin J (2017). "Colon cancer cell treatment with rose bengal generates a protective immune response via immunogenic cell death". Cell Death and Disease. 8 (2): e2584. doi:10.1038/cddis.2016.473. PMC 5386459. PMID 28151483.
- ^ Salber D, et al. (2006). "Differential uptake of [18F]FET and [3H]l-methionine in focal cortical ischemia". Nuclear Medicine and Biology. 33 (8): 1029–1035. doi:10.1016/j.nucmedbio.2006.09.004. PMID 17127177.
- ^ Watson BD, Dietrich WD, Busto R, Wachtel MS, Ginsberg MD (1985). "Induction of reproducible brain infarction by photochemically initiated thrombosis". Ann Neurol. 17 (5): 497–504. doi:10.1002/ana.410170513. PMID 4004172. S2CID 37827695.
- ^ Capinera JL, Squitier JM (2000). "Insecticidal Activity of Photoactive Dyes to American and Migratory Grasshoppers (Orthoptera: Acrididae)". Journal of Economic Entomology. 93 (3): 662–666. doi:10.1603/0022-0493-93.3.662. PMID 10902313. S2CID 25514306.
- ^ Martin P, Mischke S, Schroder R (1998). "Compatibility of Photoactive Dyes with Insect Biocontrol Agents". Biocontrol Science and Technology. 8 (4): 501–508. Bibcode:1998BioST...8..501M. doi:10.1080/09583159830018.
- ^ Feenstra R, Tseng, S (July 1992). "What is actually stained by rose bengal?". Arch Ophthalmol. 110 (7): 984–993. doi:10.1001/archopht.1992.01080190090035. PMID 1637285.
- ^ Yokoi N (2012). "Vital staining for disorders of conjunctiva and lids". Atarashii Ganka. 29: 1599–1605.
- ^ Ervin AM, Wojciechowski R, Schein O (June 26, 2017). "Punctal occlusion for dry eye syndrome". Cochrane Database Syst Rev. 9 (6): CD006775. doi:10.1002/14651858.CD006775.pub3. PMC 5568656. PMID 28649802.
- ^ Chan B, Chan O, So K (2008). "Effects of photochemical crosslinking on the microstructure of collagen and a feasibility study on controlled protein release". Acta Biomaterialia. 4 (6): 1627–1636. doi:10.1016/j.actbio.2008.06.007. PMID 18640085.
- ^ O’Neill A.C., Winograd J.M, Zeballos J.M., Johnson T.S., Randolph M.A., Bujold K.E., Kochevar I.E., Redmond R.W. (2007). "Microvascular anastomosis using a photochemical tissue bonding technique". Lasers in Surgery and Medicine. 39 (9): 716–722. doi:10.1002/lsm.20548. PMID 17960755. S2CID 46712914.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Mulroy L., Kim J., Wu I., Scharper P., Melki S.A., Azar D.A., Redmond R.W., Kochevar I.E. (2000). "Photochemical keratodesmos for repair of lamellar corneal incisions". Invest Ophthalmol Vis Sci. 41 (11): 3335–3340. PMID 11006222.
- ^ Proano C.E., Mulroy L., Erika Jones E., Azar D.A., Redmond R.W., Kochevar I.E. (2004). "Characterization of paracellular penetration routes". Invest Ophthalmol Vis Sci. 38 (11): 2177–2181. PMID 9344340.
- ^ Laser Show in the Surgical Suite, Technology Review, March/April 2009
- ^ Laser Show in the Surgical Suite, Technology Review, 02.11.2009
- ^ Walton W (1952). "Techniques for recognition of living foraminifera". Contrib. Cushman Found. Foraminiferal Res. 3: 56–60.
- ^ Panzarini E, Inguscio V, Fimia GM, Dini L (2014). "Rose Bengal acetate photodynamic therapy (RBAc-PDT) induces exposure and release of Damage-Associated Molecular Patterns (DAMPs) in human HeLa cells". PLOS ONE. 9 (8): e105778. Bibcode:2014PLoSO...9j5778P. doi:10.1371/journal.pone.0105778. PMC 4139382. PMID 25140900.
External links
[edit]- Rose+Bengal at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
- Absorption and extinction data
