User:Hamiltonstone/Sandbox2
Aged care in Australia
Background
[edit]The number and proportion of Australians aged over 65 is projected to rise... The number aged over 85 was 0.4 million in 2010, but is predicted to rise to 1.8 million by 2050, at which point it will represent 5.1 percent of the population.[1]
At the same time as the numbers of people requiring aged care being set to rise, the number of people in the workforce as a whole is projected to fall. As of 2010 there are five people of working age for every person over 65, but that will fall to around 2.7 by 2050.[2]
Provision of care
[edit]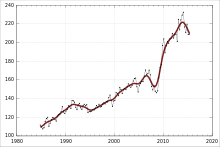
Aged care in Australia is designed to make sure that every Australian contributes toward their cost of care, depending on their individual income and assets.[3] This means that residents pay what they can afford, and the Commonwealth government pays what a resident cannot. An Australian statutory authority, the Productivity Commission, conducted a review of aged care commencing in 2010 and reporting in 2011. That review concluded that approximately 80% of care for older Australians is informal care provided by family, friends and neighbours. Around a million people received government-subsidised aged care services, most of these receiving low-level community care support, with 160 000 people in permanent residential care. Expenditure on aged care by all governments in 2009–10 was approximately $11 billion.[4]
The need for increasing amounts of care, and known weakneses in the care system (such as skilled workforce shortages and rationing of available care places), led several reviews in the 2000s to conclude that Australia's aged care system needed reform. Under a 2013 legislative and budgetary package, called Living Longer Living Better, financial assistance was provided in accordance with assessed care needs, with additional supplements available for people experiencing homelessness, dementia and veterans.[5]
Industry structure
[edit]Aged care in Australia is provided by a mix of for-profit and not-for-profit providers.
Residential care
[edit]According to the Aged Care Financing Authority, by 2013 the number of residential care beds had risen to just over 180,000, with around 60 percent provided by not-for-profit organisations, 30 percent by for-profits, and ten percent by governments.[6]
For-profit residential aged care providers include the largest, Bupa, which in 2014 had 62 facilities with 5800 residents;[7] the second-largest, Opal (formerly Domain Principal), which in 2014 operated 56 nursing homes with 4500 residents; Ality (owned by Archer Capital), and Quadrant Private Equity, as well as listed public company Japara Healthcare.[8]
Not-for-profits include Catholic aged care providers, which in 2012 provided 19,000 residential aged care beds.[9]
A person moving into residential aged care has their income and assets assessed to determine the balance of contributions that will be made by them and by government. those residents with sufficient financial means are required to pay a bond to the aged care provider. This bond is repaid when the resident moves out of aged care, but in the interim interest earned on the bond is kept by the provider, while the capital created by the pool of bonds can be used to fund capital works.[10]
In 2012–13, residential aged care was funded through a combination of national government funds (about 70 percent) and care fees paid by residents (about 25 percent), with the residual amount coming from accommodation payments or the withdrawal of small amounts from bonds paid by residents (which is permitted under the system for regulating aged care).[10]
Home care
[edit]Aged care is increasingly occurring in the home, and demand for home care support is strong. Much home care is provided by informal carers, such as family. Historically, government-supported care has been of two types: Home and Community Care (HACC) programs, which support well over half a million people; and home care packages, of which there were around 60,000 in 2012–13.[11] The packages included some that were specialised to ensure that people with dementia could receive appropriate care without having to me moved to specialised residential facilities or to hospital.
Specialised care
[edit]Dementia care
[edit]Dementia care is provided within mainstream aged care facilities, as well as specialised dementia care operations. The Australian government provides a supplementary payment to support care of individuals with dementia.
Behaviour management of people with dementia is often achieved using restraints, including psychotropic drugs. Restraints are used in many cases, and several reviews have concluded that the rate of use of restraints, particupaly antipsychotic drugs, is excessive and may be causing premature death of patients.[12] Academics[13] and advocacy organisations are seeking reduced rates of prescribing in favour of better care practices.
Palliative care
[edit]References
[edit]- ^ Productivity Commission 2011, p. xxii.
- ^ Productivity Commission 2011, p. xxx.
- ^ "Help with aged care homes". Aged care Australia. Department of Health and Ageing. Archived from the original on 2013-05-13. Retrieved 24 June 2014.
- ^ Productivity Commission 2011, p. xx.
- ^ Government, Australia. "Living Longer, Living Better – legislative changes". Department of Health and Ageing. Australian Government. Retrieved 12 July 2013.
- ^ ACFA 2013, p. 8.
- ^ "Bupa / About us / Who we are". Bupa Care Services. Retrieved 24 June 2014.
- ^ Carter, Bridget (6 June 2014). "Guilt, grief and profits in the aged-care sector". The Australian. p. 21.
- ^ "About \ The Sector". Catholic Health Australia. 2012. Retrieved 24 June 2014.
- ^ a b ACFA 2013, p. 9.
- ^ ACFA 2013, pp. 11–12.
- ^ Westbury, Juanita (9 April 2014). "Antipsychotic drugs harm older people, let's reduce their use". The Conversation. Retrieved 7 June 2014.
- ^ Hollingworth, Samantha (2011). "Psychiatric drug prescribing in elderly Australians: time for action". Australian and New Zealand Journal of Psychiatry. 45 (9): 705–708. doi:10.3109/00048674.2011.594947. PMID 21827343.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help)
Bibliography
[edit]- Productivity Commission (2011). Caring for Older Australians: Overview (PDF). Canberra: Productivity Commission.
- ACFA (30 June 2013). Inaugural Report on the funding and financing of the Aged Care Sector. Aged Care Financing Authority.
