User:Hbarton3/Cannabidiol Effects on Epilepsy
| This article is currently the subject of an educational assignment. |
 | |
 | |
| Clinical data | |
|---|---|
| AHFS/Drugs.com | International Drug Names |
| ATC code |
|
| Legal status | |
| Legal status |
Schedule II (Can) (THC - Schedule/Level I; THC and CBD two main chemicals in cannabis) |
| Pharmacokinetic data | |
| Bioavailability | 13-19% (oral)[1] |
| Elimination half-life | 9 h[1] |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| ChemSpider | |
| UNII | |
| Chemical and physical data | |
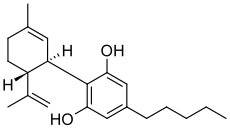
| Formula | C21H30O2 |
| Molar mass | 314.4636 g·mol−1 |
| 3D model (JSmol) | |
| Melting point | 66 °C (151 °F) |
| Boiling point | 180 °C (356 °F) (range: 160–180 °C)[2] |
| |
| |
| (verify) | |
Cannabidiol (CBD) is usually thought of as the illegal drug marijuana. Whether or not one is for or against it, recently it has been discovered that there are numerous health benefits that THC has when used properly. One case in particular that went viral deals with a young girl named Charlotte Figi who suffered from severe epilepsy and through treatments using Cannabidiol, her seizure frequency went from hundreds per week, to only a few per month. Cannabidiol has known medical uses and one of the most researched areas deals with epilepsy. [3] Cannabidiol lacks the psychotomimetic and psychotropic effects that THC entails, and it fact antagonizes these effects.[4] A study conducted in 2010 discovered that strains of cannabis containing higher concentrations of cannabidiol did not produce short-term memory impairment vs. strains with similar concentrations of THC, but lower concentrations of CBD.[5] While there is not a surplus of research on this exact situation, there is plenty of research that directly relates to it.
History
[edit]While the use a cannabis has been traced back for thousands of years, the use of cannabis for medicinal purposes is a fairly new field. Although the anticonvulsive properties of CBD have been known since the early eighties, only a few recent papers have addressed its use in samples affected with epileptic disorders. The major reasons for the lack of clinical research have been the introduction of new synthetic and more stable pharmaceutical anticonvulsants, the recognition of important adverse effects and the legal restriction to the use of cannabis-derived medicines. [6] .
Cannabidiol Receptors
[edit]There are two types of receptors that respond to cannabidiol: CB1 and CB2 receptors.
CB1 receptors
[edit]CB1 receptors are one of the most widely expressed G protein-coupled receptors in the brain. This is due to a very common form of short-term plasticity in which a single neuron is depolarized which induces a reduction in GABA-mediated neurotransmission. Endocannabinoids released from the depolarized post-synaptic neuron bind to CB1 receptors in the pre-synaptic neuron which decreases the amount of GABA secreated [7].
CB2 receptors
[edit]CB2 receptors are mainly expressed on T cells, macrophages, B cells, and in hematopoietic cells. They also have a function in keratinocytes.[8]While its role throughout the body isn't completely understood, the role that we understand the most deals with pain relief. When it comes to treating epilepsy, this is the receptor that plays the biggest role. Activation of the CB2 reduces the frequency and severity of seizures. [9]
Activation of Receptors
[edit]Currently there are drugs on the market that use the positive benefits of direct cannabinoid receptor activation. These drugs help alleviate pain in patients with advanced stages of cancer and can even help maintain a healthy body weight in AIDs patients who undergo drastic weight loss. Again while these drugs do greatly increase the quality of patients’ lives, there are some adverse side effects. Most of these adverse side effects occur due to the activation of CB1 receptors within the blood brain barrier[10]. There is little to no evidence that activation of the CB2 receptor causes any negative side effects. There is also evidence that CB2 receptor activation can relieve neuroinflammation by protecting the blood-brain and blood-spinal cord barriers. The same research shows that activation of these receptors can reduce inflammation following spinal cord injury by lowering the expression of toll-like receptors[11] .
Chemistry
[edit]The way THC and CBD interact with one another is very interesting. One would think that they have similar binding affinities and act upon the body in similar manners, however this is not the case. Typically when medicinal cannabis is grown, it is either high in THC or high in CBD. This is because CBD antagonizes the effects of THC.[12][13]
THC acts as a partial agonist at both the CB1 and CB2 human cannabinoid receptors, which are found predominantly at nerve terminals, where they have a role in retrograde regulation of synaptic function which may modulate the effects of neurotransmitters (e.g. reduce effects of excitatory neurotransmitters such as glutamate).[14]
Cannabidiol has a role in calcium homeostasis and is an inhibitor of adenosine uptake, acting largely independently of known cannabinoid receptors; it also has the potential to modulate the anxiogenic and psychoactive effects of THC.[15]
Pharmacology
[edit]Cannabidiol has a very low affinity for CB1 and CB2 receptors but acts as an indirect antagonist of their agonists.[16] While one would assume that this would cause cannabidiol to reduce the effects of THC, it may potentiate THC's effects by increasing CB1 receptor density or through another CB1-related mechanism.[17] It is also an inverse agonist of CB2 receptors.[16] Recently, it was found to be an antagonist at the putative new cannabinoid receptor, GPR55, a GPCR expressed in the caudate nucleus and putamen.[18] Cannabidiol has also been shown to act as a 5-HT1A receptor|5-HT1A receptor agonist,[19] an action which is involved in its antidepressant,[20][21] anxiolytic,[21][22] and neuroprotective[23][24] effects. Cannabidiol is an allosteric modulator of μ and δ-opioid receptors.[25] Cannabidiol's pharmacologial effects have also been attributed to PPAR-γ receptor agonism and intracellular calcium release.[26]
Charlotte Figi
[edit]Charlotte Figi was born on October 18, 2006 and when she was three months old, she had her first seizure. Some time later she was finally diagnosed with Dravet Syndrome. Dravet syndrome, also known as Severe Myoclonic Epilepsy of Infancy (SMEI), is a rare and catastrophic form of intractable epilepsy that begins in infancy. Initial seizures are most often prolonged events and in the second year of life other seizure types begin to emerge. Development remains on track initially, with plateaus and a progressive decline typically beginning in the second year of life.
The only solution that her parents could find dealt with using medical marijuana that is high in CBD and low in THC. They followed the necessary steps in order to get Charlotte on the medical marijuana registry. The average age of patients on the registry is forty two and there are only ninety under the age of eighteen[27]. Dr. Margaret Gedde and Dr. Alan Shackelford were the two physicians who signed off on Charlotte's papers. As soon as they could, Charlotte's parents made their first buy of a strand that was high in cannabidiol and low in THC.
In order to avoid smoking marijuana, one can extract the oil. This is a common practice when one wants to add THC or CBD to food. When the oil is extracted, it can be used to cook or directly applied to food. Charlotte's parents started by adding 3mg of the oil to her food. Charlotte had been having around 300 seizures a week and for the first time in years she was seizure free for a couple hours. The next step was to find a reliable source of marijuana that was high in CBD and low in THC. The Figis found the Stanleys. The Stanley Brothers are one of the largest medical marijuana dispensers and growers in the state of Colorado and they speicliaze in strands that are high in CBD and low in THC.[28] This viral story was very important in the fight to raise awareness and funds for research dealing with medical marijuana.
Publicity
[edit]This area of research typically gets negative feedback from the public. This is an expected problem when dealing with a substance that is illegal in most countries. The biggest problem is convincing people that the research being done is medically related and can potentially help cure man neurological disorders. There are companys that are currently working on medications that are high in CBD and low in THC to treat an assortment of disorders. One of these is Sativex. Sativex was developed by GW Pharmaceuticals a British biopharmaceutical company. Sativex is an oral spray used to treat patients with multiple sclerosis but has the potential to be used in other neuro-degenerative disorders. Developments such as this help to desensitize the public to the use of medicinal cannabis. Other ways that help this matter are when well known scientists come out and back the use of medicinal cannabis. One such historical case of this just recently occurred. Dr. Sanjay Gupta is an American neurosurgeon and an assistant professor of neurosurgery at Emory University School of Medicine and associate chief of the neurosurgery service at Grady Memorial Hospital in Atlanta, Georgia. In the past he has been a strong advocate against the use of medical cannabis, however, after the Charlotte Figi case went viral, Dr. Gupta changed his mind. He came out and apologized for his previous stance and now believes that we should be putting more time and effort into developing cures to diseases using the power of cannabidiol.
References
[edit]- ^ a b Mechoulam, R; Parker, LA; Gallily, R (November 2002). "Cannabidiol: an overview of some pharmacological aspects". Journal of Clinical Pharmacology. 42 (11 Suppl): 11S–19S. doi:10.1002/j.1552-4604.2002.tb05998.x. PMID 12412831. S2CID 10024088.
- ^ McPartland, JM; Russo, EB (2001). "Cannabis and Cannabis Extracts: Greater Than the Sum of Their Parts?" (PDF). Journal of Cannabis Therapeutics. 1 (3/4): 103–132. doi:10.1300/J175v01n03_08.
- ^ Jones, N, A. (2012). "Cannabidiol exerts anti-convulsant effects in animal models of temporal lobe and partial seizures". Seizure. 21 (5): 344–352. doi:10.1016/j.seizure.2012.03.001. PMID 22520455. S2CID 2819823.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help)CS1 maint: multiple names: authors list (link) - ^ Campos, A.C. (2012). "Multiple mechanisms involved in the large-spectrum therapeutic potential of cannabidiol in psychiatric disorders". Philos Trans R Soc Lond B Biol Sci. 367 (1607): 3364–3378. doi:10.1098/rstb.2011.0389. PMC 3481531. PMID 23108553.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Frood, A. (2010). "Key ingredient staves off marijuana memory loss". Nature. doi:10.1038/news.2010.508.
- ^ Pertwee, R.G. (2012). "Targeting the endocannabinoid system with cannabinoid receptor agonists: pharmacological strategies and therapeutic possibilities". Philosophical Transactions of the Royal Society B-Biological Sciences. 367 (1607): 3353–3363. doi:10.1098/rstb.2011.0381. PMC 3481523. PMID 23108552.
- ^ "The endocannabinoid-CB1 receptor system in pre- and postnatal life" - Ester Fride, "European Journal of Pharmacology" (Volume 500, Issues 1–3, 1 October 2004, Pages 289–297)
- ^ Pacher P, Mechoulam R (2011). "Is lipid signaling through cannabinoid 2 receptors part of a protective system?". Prog Lipid Res. 50 (2): 193–211. doi:10.1016/j.plipres.2011.01.001. PMC 3062638. PMID 21295074.
- ^ Basu, S.; Ray, A.; Dittel, B. N. (2011). "Cannabinoid Receptor 2 (CB2) is Critical for the Homing and Retention of Marginal Zone B Lineage Cells and for Efficient T-independent Immune Responses". The Journal of Immunology. 187 (11): 5720–5732. doi:10.4049/jimmunol.1102195. PMC 3226756. PMID 22048769.
- ^ Robson, P.J. (2014). "Therapeutic potential of cannabinoid medicines". Drug Test Anal. 6 (1–2): 24–30. doi:10.1002/dta.1529. PMID 24006213.
- ^ Pertwee, R.G. (2012). "Targeting the endocannabinoid system with cannabinoid receptor agonists: pharmacological strategies and therapeutic possibilities". Philosophical Transactions of the Royal Society B-Biological Sciences. 367 (1607): 3353–3363. doi:10.1098/rstb.2011.0381. PMC 3481523. PMID 23108552.
- ^ Robson, P.J. (2014). "Therapeutic potential of cannabinoid medicines". Drug Test Anal. 6 (1–2): 24–30. doi:10.1002/dta.1529. PMID 24006213.
- ^ Pertwee, R.G. (2012). "Targeting the endocannabinoid system with cannabinoid receptor agonists: pharmacological strategies and therapeutic possibilities". Philosophical Transactions of the Royal Society B-Biological Sciences. 367 (1607): 3353–3363. doi:10.1098/rstb.2011.0381. PMC 3481523. PMID 23108552.
- ^ Ryan, D (2009). "Cannabidiol targets mitochondria to regulate intracellular Ca2+ levels". J Neurosci. 29 (7): 2053–2063. doi:10.1523/JNEUROSCI.4212-08.2009. PMC 6666323. PMID 19228959.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Karniol, IG (1973). "Pharmacological Interaction between Cannabidiol and Δ9-Tetrahydrocannabinol". Psychopharmacologia. 33 (1): 53–70. doi:10.1007/BF00428793. PMID 4358666. S2CID 26006265.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ a b Pertwee, R. G. (2008). "The diverse CB1 and CB2 receptor pharmacology of three plant cannabinoids: Δ9-tetrahydrocannabinol, cannabidiol and Δ9-tetrahydrocannabivarin". British Journal of Pharmacology. 153 (2): 199–215. doi:10.1038/sj.bjp.0707442. PMC 2219532. PMID 17828291.
- ^ Hayakawa, K.; Mishima, K.; Hazekawa, M.; Sano, K.; Irie, K.; Orito, K.; Egawa, T.; Kitamura, Y.; Uchida, N.; Nishimura, R.; Egashira, N.; Iwasaki, K.; Fujiwara, M. (2008). "Cannabidiol potentiates pharmacological effects of Δ9-tetrahydrocannabinol via CB1 receptor-dependent mechanism". Brain Research. 1188: 157–164. doi:10.1016/j.brainres.2007.09.090. PMID 18021759. S2CID 25082053.
- ^ Ryberg E; Larsson N; Sjögren S; et al. (2007). "The orphan receptor GPR55 is a novel cannabinoid receptor". British Journal of Pharmacology. 152 (7): 1092–101. doi:10.1038/sj.bjp.0707460. PMC 2095107. PMID 17876302.
{{cite journal}}: Explicit use of et al. in:|author4=(help) - ^ Russo EB, Burnett A, Hall B, Parker KK (2005). "Agonistic properties of cannabidiol at 5-HT1a receptors". Neurochemical Research. 30 (8): 1037–43. doi:10.1007/s11064-005-6978-1. PMID 16258853. S2CID 207222631.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Zanelati, T; Biojone, C; Moreira, F; Guimarães, F; Joca, S (2010). "Antidepressant-like effects of cannabidiol in mice: possible involvement of 5-HT1A receptors". British Journal of Pharmacology. 159 (1): 122–8. doi:10.1111/j.1476-5381.2009.00521.x. PMC 2823358. PMID 20002102.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b Resstel LB, Tavares RF, Lisboa SF, Joca SR, Corrêa FM, Guimarães FS (2009). "5-HT1A receptors are involved in the cannabidiol-induced attenuation of behavioural and cardiovascular responses to acute restraint stress in rats". British Journal of Pharmacology. 156 (1): 181–8. doi:10.1111/j.1476-5381.2008.00046.x. PMC 2697769. PMID 19133999.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Campos AC, Guimarães FS (2008). "Involvement of 5HT1A receptors in the anxiolytic-like effects of cannabidiol injected into the dorsolateral periaqueductal gray of rats". Psychopharmacology. 199 (2): 223–30. doi:10.1007/s00213-008-1168-x. PMID 18446323. S2CID 22749049.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Mishima K; Hayakawa K; Abe K; et al. (2005). "Cannabidiol prevents cerebral infarction via a serotonergic 5-hydroxytryptamine1A receptor-dependent mechanism". Stroke; A Journal of Cerebral Circulation. 36 (5): 1077–82. doi:10.1161/01.STR.0000163083.59201.34. PMID 15845890. S2CID 6806707.
{{cite journal}}: Explicit use of et al. in:|author4=(help); Unknown parameter|month=ignored (help) - ^ Hayakawa K; Mishima K; Nozako M; et al. (2007). "Repeated treatment with cannabidiol but not Delta9-tetrahydrocannabinol has a neuroprotective effect without the development of tolerance". Neuropharmacology. 52 (4): 1079–87. doi:10.1016/j.neuropharm.2006.11.005. PMID 17320118. S2CID 23816947.
{{cite journal}}: Explicit use of et al. in:|author4=(help); Unknown parameter|month=ignored (help) - ^ Kathmann, Markus; Flau, Karsten; Redmer, Agnes; Tränkle, Christian; Schlicker, Eberhard (2006). "Cannabidiol is an allosteric modulator at mu- and delta-opioid receptors". Naunyn-Schmiedeberg's Archives of Pharmacology. 372 (5): 354–361. doi:10.1007/s00210-006-0033-x. PMID 16489449. S2CID 4877869.
- ^ Campos, A. C.; Moreira, F. A.; Gomes, F. V.; Del Bel, E. A.; Guimaraes, F. S. (2012). "Multiple mechanisms involved in the large-spectrum therapeutic potential of cannabidiol in psychiatric disorders". Philosophical Transactions of the Royal Society B: Biological Sciences. 367 (1607): 3364–3378. doi:10.1098/rstb.2011.0389. PMC 3481531. PMID 23108553.
- ^ "Medical Marijuana Statistics". Colorado Department of Public Health and Environment. Retrieved 10 December 2013.
- ^ http://www.cnn.com/2013/08/07/health/charlotte-child-medical-marijuana/
