User:Jolivia03
Acne Cosmetica, also known as "Acne due to Cosmetics" and "Cosmetic-Induced Acne," is a condition that occurs due to the use of certain makeup and beauty products. It is a term that was first coined in 1972 by dermatologist Albert M. Kligman to represent the post-adolescent acne they believed was caused by cosmetic use [1]. As the name suggests, acne cosmetica is a form of acne triggered by the use of cosmetic products [1]. This is certainly not limited to makeup, as any products applied to the face and the surrounding areas can instigate this type of breakouts. Products in the surrounding areas of the face include but are not limited to hair gels, conditioners, etc. This condition can occur in males or females, and even those not previously predisposed to acne breakouts. Acne cosmetica affects areas like the cheeks and forehead where cosmetics, hair care products, and lotions are most frequently applied [2]. The condition develops over a period of weeks or months and appears as small, itchy, or rash-like pink bumps. If changes in product use, hygiene practices, or application techniques are not altered, the condition may persist indefinitely [2].
Signs and symptoms
[edit]Acne Cosmetica may have a slow onset. In some cases, the appearance of the signs and symptoms is not immediate after usage of the makeup or topical beauty product[2]. With that being said, it may take days, weeks, and months for the lesions to develop. The signs and symptoms of acne cosmetic include: The pimples develop on the areas of application, which may include the face and neck (mostly), chest, back, and legs.
- (In many cases) the condition is mild and small bumps may seen
- Prolonged use of the offending cosmetic may cause severe skin lesion
- Individuals with existing acne may have more severe condition
- Individuals with existing acne may have more severe condition
Causes
[edit]This type of acne is caused by the use of comedogenic hair or skin care products. Comedogenic hair and skin care products and makeup are the cause of acne cosmetica. Comedogenic simply means a product that aggravates or causes acne in the skin. These types of cosmetics build-up in the follicle and block the pore. When the pore is blocked, skin oil builds up and a comedone appears on the skin. Excess skin oil builds up, clogging the pore and creating a blemish. Pomades or hair oils, heavy moisturizers, eye creams, and makeup are all common causes of acne cosmetica.
Mechanism / Pathophysiology
[edit]
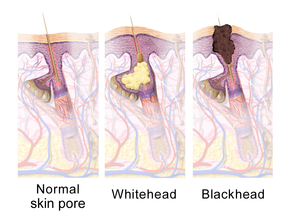

The mechanism of Acne Cosmetica was presumably a chemically induced plugging of the pilosebaceous orifice. This became a significant problem for dermatologists in the 1970s and 1980s, but with the improved formulations produced by cosmetic chemists over the past thirty years, a diagnosis of acne cosmetica has become relatively rare daily dermatological practice. It is considered a trigger to "basic" acne caused by several (topical) beauty products. Acne Cosmetica is typically not a serious medical condition. However, it can lead to unsightly and sometimes painful lesions and ultimately scars. When pimples are open, the skin barrier has been disrupted. Any makeup applied to the area can then get into deeper levels of exposed tissue than the product is designed to reach. The result can be added irritation with increased redness and swelling of the pimple[2].
Diagnosis
[edit]Acne Cosmetica is diagnosed through a simple physical examination by the physician or a dermatologist. The healthcare provider may ask several questions related to the individual’s age, family medical history, current medications, cosmetics, body lotions used, other medical conditions, infections, etc. If secondary infections develop, then a culture test may be done. Invasive methods, such as skin biopsy, are typically not required; a diagnosis of acne can be made through a physical examination itself [2].
Treatment
[edit]It is important to immediately discontinue the use of the comedogenic product and replace with a non-comedogenic makeup in order to improve the skin’s condition. The use of antiseptic, antibiotic topical applications, anti-inflammatory gels, lotions and creams such as benzoyl peroxide and salicylic acid will be beneficial. If infections occur, medications such as antibiotics may be used. In case of severe acne, isotretinoin is prescribed (though, NOT for pregnant women). However, there may be some adverse side effects for this drug, and therefore close monitoring is requested.
Another treatment method for Acne Cosmetica is called dermabrasion and is performed under local anesthesia. In this procedure, the raised lumpy acne scars and skin dark spots are abraded. There are other cosmetic procedures such as, chemical peeling, minor skin surgery (punch excision), and microdermabrasion, which may be used.
Further treatment options include phototherapy, which is a controlled exposure to light for a certain time duration; however, this method is not very effective for long-lasting acne. Surgical procedures using laser are also used as forms of treatment for Acne Cosmetica.
Ultimately, Taking care of oneself, being clean and hygienic (especially face and hands), avoiding the urge to touch/break the blisters, avoiding oily make-ups and creams, drinking lots of water, etc. are all simple practices that can ensure a faster recovery from Acne Cosmetica [2].
Most treatments methods for Acne Cosmetica are parallel to the medications used in the treatment of Acne Vulgaris.
Medications
[edit]Benzoyl peroxide
[edit]
Benzoyl peroxide (BPO) is a first-line treatment for mild and moderate acne due to its effectiveness and mild side-effects (mainly skin irritation). In the skin follicle, benzoyl peroxide kills C. acnes by oxidizing its proteins through the formation of oxygen free radicals and benzoic acid. These free radicals are thought to interfere with the bacterium's metabolism and ability to make proteins.[3][4] Additionally, benzoyl peroxide is mildly effective at breaking down comedones and inhibiting inflammation.[5][4] Benzoyl peroxide may be paired with a topical antibiotic or retinoid such as benzoyl peroxide/clindamycin and benzoyl peroxide/adapalene, respectively.[6]
Side effects include increased skin photosensitivity, dryness, redness and occasional peeling.[7] Sunscreen use is often advised during treatment, to prevent sunburn. Lower concentrations of benzoyl peroxide are just as effective as higher concentrations in treating acne but are associated with fewer side effects.[4][8] Unlike antibiotics, benzoyl peroxide does not appear to generate bacterial antibiotic resistance.[7]
Salicylic acid
Salicylic acid is a topically applied beta-hydroxy acid that stops bacteria from reproducing and has keratolytic properties.[9][10] It opens obstructed skin pores and promotes shedding of epithelial skin cells.[9] Salicylic acid is known to be less effective than retinoid therapy.[11] Dry skin is the most commonly seen side effect with topical application, though darkening of the skin has been observed in individuals with darker skin types.[12]
Antibiotics
[edit]Antibiotics are frequently applied to the skin or taken orally to treat acne and are thought to work due to their antimicrobial activity against C. acnes and their ability to reduce inflammation.[11][7][13] With the widespread use of antibiotics for acne and an increased frequency of antibiotic-resistant C. acnes worldwide, antibiotics are becoming less effective,[7] especially macrolide antibiotics such as topical erythromycin.[14][13] Therefore, they are not recommended for use alone but are preferred as part of combination therapy.[15] Commonly used antibiotics, either applied to the skin or taken orally, include clindamycin, erythromycin, metronidazole, sulfacetamide, and tetracyclines such as doxycycline and minocycline.[16] Doxycycline 40 milligrams daily (low-dose) appears to have similar efficacy to doxycycline 100 milligrams daily and has fewer gastrointestinal side effects.[15] When antibiotics are applied to the skin, they are typically used for mild to moderately severe acne.[11] Antibiotics taken orally are generally considered to be more effective than topical antibiotics, and produce faster resolution of inflammatory acne lesions than topical applications.[12] Topical and oral antibiotics are not recommended for use together.[13]
Oral antibiotics are recommended for no longer than three months as antibiotic courses exceeding this duration are associated with the development of antibiotic resistance and show no clear benefit over shorter courses.[13] Furthermore, if long-term oral antibiotics beyond three months are thought to be necessary, it is recommended that benzoyl peroxide and/or a retinoid be used at the same time to limit the risk of C. acnes developing antibiotic resistance.[13]
Dapsone has shown efficacy against inflammatory acne but is generally not a first-line topical antibiotic due to higher cost and lack of clear superiority over other antibiotics.[12][15] It is sometimes a preferred therapy in women or for people with sensitive or darker toned skin.[15] Topical dapsone is not recommended for use with benzoyl peroxide due to yellow-orange skin discoloration with this combination.[17] While minocycline is shown to be an effective acne treatment, it is no longer recommended as a first-line antibiotic due to a lack of evidence that it is better than other treatments, and concerns of safety compared to other tetracyclines.[18]
Combination therapy
[edit]Combination therapy—using medications of different classes together, each with a different mechanism of action—has been demonstrated to be a more efficacious approach to acne treatment than monotherapy.[17][16] The use of topical benzoyl peroxide and antibiotics together has been shown to be more effective than antibiotics alone.[17] Similarly, using a topical retinoid with an antibiotic clears acne lesions faster than the use of antibiotics alone.[17] Frequently used combinations include the following: antibiotic and benzoyl peroxide, antibiotic and topical retinoid, or topical retinoid and benzoyl peroxide.[16] The pairing of benzoyl peroxide with a retinoid is preferred over the combination of a topical antibiotic with a retinoid since both regimens are effective but benzoyl peroxide does not lead to antibiotic resistance.[17]
Professional Treatments
[edit]If limiting the use of cosmetics does not work, and ones acne breakouts/blemishes becomes uncontrollable, Comedo extraction is supported by limited evidence but is recommended for comedones that do not improve with standard treatment.[19][5] Another procedure for immediate relief is injection of a corticosteroid into an inflamed acne comedo.[5] Electrocautery and electrofulguration have also been reported as effective treatments for comedones.[20]
Light therapy is a treatment method that involves delivering certain specific wavelengths of light to an area of skin affected by acne. Both regular and laser light have been used. The evidence for light therapy as a treatment for acne is weak and inconclusive.[19][21] Various light therapies appear to provide a short-term benefit, but data for long-term outcomes, and for outcomes in those with severe acne, are sparse;[22] it may have a role for individuals whose acne has been resistant to topical medications.[17] A 2016 meta-analysis was unable to conclude whether light therapies were more beneficial than placebo or no treatment, nor how long potential benefits lasted.[23] PDT has the most supporting evidence of all light therapies.[5]
When regular light is used immediately following the application of a sensitizing substance to the skin such as aminolevulinic acid or methyl aminolevulinate, the treatment is referred to as photodynamic therapy (PDT).[17][24] Many different types of nonablative lasers (i.e., lasers that do not vaporize the top layer of the skin but rather induce a physiologic response in the skin from the light) have been used to treat acne, including those that use infrared wavelengths of light. Ablative lasers (such as CO2 and fractional types) have also been used to treat active acne and its scars. When ablative lasers are used, the treatment is often referred to as laser resurfacing because, as mentioned previously, the entire upper layers of the skin are vaporized.[25] Ablative lasers are associated with higher rates of adverse effects compared with nonablative lasers, with examples being postinflammatory hyperpigmentation, persistent facial redness, and persistent pain.[19][26][27] Physiologically, certain wavelengths of light, used with or without accompanying topical chemicals, are thought to kill bacteria and decrease the size and activity of the glands that produce sebum.[24] Disadvantages of light therapy can include its cost, the need for multiple visits, time required to complete the procedure(s), and pain associated with some of the treatment modalities.[17] Typical side effects include skin peeling, temporary reddening of the skin, swelling, and postinflammatory hyperpigmentation.[17]
Dermabrasion is an effective therapeutic procedure for reducing the appearance of superficial atrophic scars of the boxcar and rolling varieties.[28] Ice-pick scars do not respond well to treatment with dermabrasion due to their depth.[28] The procedure is painful and has many potential side effects such as skin sensitivity to sunlight, redness, and decreased pigmentation of the skin.[28] Dermabrasion has fallen out of favor with the introduction of laser resurfacing.[28] Unlike dermabrasion, there is no evidence that microdermabrasion is an effective treatment for acne.[19]
Dermal or subcutaneous fillers are substances injected into the skin to improve the appearance of acne scars. Fillers are used to increase natural collagen production in the skin and to increase skin volume and decrease the depth of acne scars.[29] Examples of fillers used for this purpose include hyaluronic acid; poly(methyl methacrylate) microspheres with collagen; human and bovine collagen derivatives, and fat harvested from the person's own body (autologous fat transfer).[29]
Microneedling is a procedure in which an instrument with multiple rows of tiny needles is rolled over the skin to elicit a wound healing response and stimulate collagen production to reduce the appearance of atrophic acne scars in people with darker skin color.[25] Notable adverse effects of microneedling include postinflammatory hyperpigmentation and tram track scarring (described as discrete slightly raised scars in a linear distribution similar to a tram track). The latter is thought to be primarily attributable to improper technique by the practitioner, including the use of excessive pressure or inappropriately large needles.[25][30]
Subcision is useful for treatment of superficial atrophic acne scars and involves the use of a small needle to loosen the fibrotic adhesions that result in the depressed appearance of the scar.[31][32][33]
Chemical peels can be used to reduce the appearance of acne scars.[28] Mild peels include those using glycolic acid, lactic acid, salicylic acid, Jessner's solution, or a lower concentrations (20%) of trichloroacetic acid. These peels only affect the epidermal layer of the skin and can be useful in the treatment of superficial acne scars as well as skin pigmentation changes from inflammatory acne.[28] Higher concentrations of trichloroacetic acid (30–40%) are considered to be medium-strength peels and affect skin as deep as the papillary dermis.[28] Formulations of trichloroacetic acid concentrated to 50% or more are considered to be deep chemical peels.[28] Medium-strength and deep-strength chemical peels are more effective for deeper atrophic scars, but are more likely to cause side effects such as skin pigmentation changes, infection, and small white superficial cysts known as milia.[28]
Prognosis
[edit]The prognosis of Acne Cosmetica depends upon the severity of the signs and symptoms[2]. In general, the prognosis is excellent with appropriate treatment. In many cases, the signs and symptoms improve following stoppage of the cosmetic product causing acne and with adequate treatment [2]
Epidemiology
[edit]Similar to Acne Vulgaris, Acne Cosmetica globally affects approximately 650 million people, or about 9.4% of the population, as of 2010.[34] It affects nearly 90% of people in Western societies during their teenage years, and may persist into adulthood if not treated.[35][11][36] It is slightly more common in females than males (9.8% versus 9.0%) being that women apply makeup significantly more than men.[34] Research has found that it affects people of all ethnic groups[37].

Research
[edit]As research involving the study of Acne Cosmetica are slim, a case study was conducted in the Department of Dermatology and Venereology and Medicine and the Institute of Medical Sciences to examine the association of post-adolescent acne with the use of cosmetics and cosmetic procedures [38]. Comparison of different cumulative exposure categories with the lowest exposure category (multivariate analysis, logistic regression) showed that the odds ratios, which were always <1, progressively declined as cosmetic exposure increased [odds ratios (95% confidence intervals): 0.679 (0.501-0.922), 0.355 (0.258-0.487), 0.307 (0.217-0.433)]. However, some individual cosmetics had odds ratios >1 [38]. As a result, the research concludes that overall cosmetic use was negatively associated with post-adolescent acne. According the the authors, the term ‘acne cosmetica' is appropriate in the sense that some cosmetics may cause acne.
References
[edit]- ^ a b M.D, Jennifer Linder. "The Truth About Acne Cosmetica". www.dermascope.com. Retrieved 2019-12-11.
- ^ a b c d e f g h www.dovemed.com https://www.dovemed.com/diseases-conditions/acne-cosmetica/. Retrieved 2019-12-11.
{{cite web}}: Missing or empty|title=(help) - ^ Leccia MT, Auffret N, Poli F, Claudel JP, Corvec S, Dreno B (August 2015). "Topical acne treatments in Europe and the issue of antimicrobial resistance". Journal of the European Academy of Dermatology and Venereology (Review). 29 (8): 1485–92. doi:10.1111/jdv.12989. PMID 25677763.
- ^ a b c Gamble R, Dunn J, Dawson A, Petersen B, McLaughlin L, Small A, et al. (June 2012). "Topical antimicrobial treatment of acne vulgaris: an evidence-based review". American Journal of Clinical Dermatology (Review). 13 (3): 141–52. doi:10.2165/11597880-000000000-00000. PMID 22268388.
- ^ a b c d Zaenglein AL, Pathy AL, Schlosser BJ, Alikhan A, Baldwin HE, Berson DS, et al. (May 2016). "Guidelines of care for the management of acne vulgaris". Journal of the American Academy of Dermatology (Review). 74 (5): 945–73.e33. doi:10.1016/j.jaad.2015.12.037. PMID 26897386.
- ^ Yin NC, McMichael AJ (February 2014). "Acne in patients with skin of color: practical management". American Journal of Clinical Dermatology (Review). 15 (1): 7–16. doi:10.1007/s40257-013-0049-1. PMID 24190453.
- ^ a b c d Sagransky M, Yentzer BA, Feldman SR (October 2009). "Benzoyl peroxide: a review of its current use in the treatment of acne vulgaris". Expert Opinion on Pharmacotherapy (Review). 10 (15): 2555–62. doi:10.1517/14656560903277228. PMID 19761357.
- ^ Brandstetter AJ, Maibach HI (August 2013). "Topical dose justification: benzoyl peroxide concentrations". The Journal of Dermatological Treatment (Review). 24 (4): 275–7. doi:10.3109/09546634.2011.641937. PMID 22103743.
- ^ a b Madan RK, Levitt J (April 2014). "A review of toxicity from topical salicylic acid preparations". Journal of the American Academy of Dermatology (Review). 70 (4): 788–792. doi:10.1016/j.jaad.2013.12.005. PMID 24472429.
- ^ Well D (October 2013). "Acne vulgaris: A review of causes and treatment options". The Nurse Practitioner (Review). 38 (10): 22–31, quiz 32. doi:10.1097/01.NPR.0000434089.88606.70. PMID 24048347.
- ^ a b c d Dawson AL, Dellavalle RP (May 2013). "Acne vulgaris". BMJ (Review). 346 (5): 30–33. doi:10.1136/bmj.f2634. JSTOR 23494950. PMID 23657180.
- ^ a b c Vary JC (November 2015). "Selected Disorders of Skin Appendages--Acne, Alopecia, Hyperhidrosis". The Medical Clinics of North America (Review). 99 (6): 1195–211. doi:10.1016/j.mcna.2015.07.003. PMID 26476248.
- ^ a b c d e Walsh TR, Efthimiou J, Dréno B (March 2016). "Systematic review of antibiotic resistance in acne: an increasing topical and oral threat" (PDF). The Lancet. Infectious Diseases (Systematic Review). 16 (3): e23-33. doi:10.1016/S1473-3099(15)00527-7. PMID 26852728.
- ^ Beylot C, Auffret N, Poli F, Claudel JP, Leccia MT, Del Giudice P, Dreno B (March 2014). "Propionibacterium acnes: an update on its role in the pathogenesis of acne". Journal of the European Academy of Dermatology and Venereology (Review). 28 (3): 271–8. doi:10.1111/jdv.12224. PMID 23905540.
- ^ a b c d Zaenglein AL (October 2018). "Acne Vulgaris". The New England Journal of Medicine (Review). 379 (14): 1343–1352. doi:10.1056/NEJMcp1702493. PMID 30281982.
- ^ a b c Kong YL, Tey HL (June 2013). "Treatment of acne vulgaris during pregnancy and lactation". Drugs (Review). 73 (8): 779–87. doi:10.1007/s40265-013-0060-0. PMID 23657872.
- ^ a b c d e f g h i Aslam I, Fleischer A, Feldman S (March 2015). "Emerging drugs for the treatment of acne". Expert Opinion on Emerging Drugs (Review). 20 (1): 91–101. doi:10.1517/14728214.2015.990373. PMID 25474485.(subscription required)
- ^ Garner SE, Eady A, Bennett C, Newton JN, Thomas K, Popescu CM (August 2012). "Minocycline for acne vulgaris: efficacy and safety". The Cochrane Database of Systematic Reviews (8): CD002086. doi:10.1002/14651858.CD002086.pub2. PMID 22895927.
- ^ a b c d Titus S, Hodge J (October 2012). "Diagnosis and treatment of acne". American Family Physician (Review). 86 (8): 734–40. PMID 23062156. Archived from the original on 18 February 2015.
- ^ Bolognia JL, Jorizzo JL (2012). Dermatology (3rd ed.). St. Louis, Mo.: Mosby Elsevier. p. 558. ISBN 9780702051821.
- ^ Posadzki P, Car J (May 2018). "Light Therapies for Acne". JAMA Dermatology. 154 (5): 597–598. doi:10.1001/jamadermatol.2018.0110. PMID 29541753.
- ^ Hamilton FL, Car J, Lyons C, Car M, Layton A, Majeed A (June 2009). "Laser and other light therapies for the treatment of acne vulgaris: systematic review". The British Journal of Dermatology (Systematic Review & Meta-Analysis). 160 (6): 1273–85. doi:10.1111/j.1365-2133.2009.09047.x. PMID 19239470.
- ^ Barbaric J, Abbott R, Posadzki P, Car M, Gunn LH, Layton AM, et al. (September 2016). "Light therapies for acne". The Cochrane Database of Systematic Reviews. 9: CD007917. doi:10.1002/14651858.CD007917.pub2. PMC 6457763. PMID 27670126.
- ^ a b Pugashetti R, Shinkai K (July 2013). "Treatment of acne vulgaris in pregnant patients". Dermatologic Therapy (Review). 26 (4): 302–11. doi:10.1111/dth.12077. PMID 23914887.
- ^ a b c Cohen BE, Elbuluk N (February 2016). "Microneedling in skin of color: A review of uses and efficacy". Journal of the American Academy of Dermatology (Review). 74 (2): 348–55. doi:10.1016/j.jaad.2015.09.024. PMID 26549251.
- ^ Ong MW, Bashir SJ (June 2012). "Fractional laser resurfacing for acne scars: a review". The British Journal of Dermatology (Review). 166 (6): 1160–9. doi:10.1111/j.1365-2133.2012.10870.x. PMID 22296284.
- ^ Abdel Hay R, Shalaby K, Zaher H, Hafez V, Chi CC, Dimitri S, et al. (April 2016). "Interventions for acne scars". The Cochrane Database of Systematic Reviews (Systematic Review & Meta-Analysis). 4: CD011946. doi:10.1002/14651858.CD011946.pub2. PMID 27038134.
- ^ a b c d e f g h i Levy LL, Zeichner JA (October 2012). "Management of acne scarring, part II: a comparative review of non-laser-based, minimally invasive approaches". American Journal of Clinical Dermatology (Review). 13 (5): 331–40. doi:10.2165/11631410-000000000-00000. PMID 22849351.
- ^ a b Soliman YS, Horowitz R, Hashim PW, Nia JK, Farberg AS, Goldenberg G (July 2018). "Update on acne scar treatment". Cutis (Review). 102 (1): 21, 25, 47, 48. PMID 30138491.
- ^ Pahwa M, Pahwa P, Zaheer A (July 2012). ""Tram track effect" after treatment of acne scars using a microneedling device". Dermatologic Surgery (Case Report & Literature Review). 38 (7 Pt 1): 1107–8. doi:10.1111/j.1524-4725.2012.02441.x. PMID 22587597.
- ^ Lanoue J, Goldenberg G (May 2015). "Acne scarring: a review of cosmetic therapies". Cutis (Review). 95 (5): 276–81. PMID 26057505.
- ^ Kroepfl L, Emer JJ (November 2016). "Combination Therapy for Acne Scarring: Personal Experience and Clinical Suggestions". Journal of Drugs in Dermatology (Review). 15 (11): 1413–1419. PMID 28095556.
- ^ Zaleski-Larsen LA, Fabi SG, McGraw T, Taylor M (May 2016). "Acne Scar Treatment: A Multimodality Approach Tailored to Scar Type". Dermatologic Surgery (Review). 42 Suppl 2 (Supplement 2): S139-49. doi:10.1097/DSS.0000000000000746. PMID 27128240.
- ^ a b Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, et al. (December 2012). "Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet. 380 (9859): 2163–96. doi:10.1016/S0140-6736(12)61729-2. PMC 6350784. PMID 23245607.
- ^ Taylor M, Gonzalez M, Porter R (May–June 2011). "Pathways to inflammation: acne pathophysiology". European Journal of Dermatology (Review). 21 (3): 323–33. doi:10.1684/ejd.2011.1357. PMID 21609898.
- ^ Admani S, Barrio VR (November 2013). "Evaluation and treatment of acne from infancy to preadolescence". Dermatologic Therapy (Review). 26 (6): 462–6. doi:10.1111/dth.12108. PMID 24552409.
- ^ Shah SK, Alexis AF (May 2010). "Acne in skin of color: practical approaches to treatment". The Journal of Dermatological Treatment (Review). 21 (3): 206–11. doi:10.3109/09546630903401496. PMID 20132053.
- ^ a b Singh, Sanjay; Mann, Baldeep Kaur; Tiwary, Narendra K. (2013). "Acne Cosmetica Revisited: A Case-Control Study Shows a Dose-Dependent Inverse Association between Overall Cosmetic Use and Post-Adolescent Acne". Dermatology. 226 (4): 337–341. doi:10.1159/000350936. ISSN 1018-8665. PMID 23859829.
