User:LittleWen/sandbox
Mucus (/ˈm[invalid input: 'ju:']kəs/ MEW-kəss) is a slippery aqueous secretion produced by, and covering, mucous membranes. It is typically produced from cells found in mucous glands, although it may also originate from mixed glands, which contain both serous and mucous cells. It is a viscous colloid containing inorganic salts, antiseptic enzymes (such as lys), immunoglobulins, and glycoproteinsoteins such as lactoferrin and mucinsns, which are produced by goblet cells in the mucous membranes and submucosal glands. Mucus serves to protect epithelial cells (that line the tubes) in the respiratory, gastrointestinal, urogenital, visual, and auditory systems; the epidermis in amphibians; and the gills in fish, against infectious agents such as fungi, bacteria and viruses. The average human nose produces about a liter of mucus per day.[1] Most of the mucus produced is in the gastrointestinal tract.
Bony fish, hagfish, snails, slugs, and some other invertebrates also produce external mucus. In addition to serving a protective function against infectious agents, such mucus provides protection against toxins produced by predators, can facilitate movement and may play a role in communication.
Respiratory system
[edit]
In the human respiratory system, mucus, also known as airway surface liquid (ASL), aids in the protection of the lungs by trapping foreign particles that enter them, in particular, through the nose, during normal breathing.[2] Further distinction exists between the superficial and cell-lining layers of ASL, which are known as mucus layer (ML) and pericilliary liquid layer (PCL), respectively.[3] "Phlegm" is a specialized term for mucus that is restricted to the respiratory tract, whereas the term "nasal mucus" describes secretions of the nasal passages.
Nasal mucus is produced by the nasal mucosa; and mucus lining the airways (trachea, bronchus, bronchioles) is produced by specialized airway epithelial cells (goblet cells) and submucosal glands. Small particles such as dust, particulate pollutants, and allergens, as well as infectious agents and bacteria are caught in the viscous nasal or airway mucus and prevented from entering the system. This event along with the continual movement of the respiratory mucus layer toward the oropharynx, helps prevent foreign objects from entering the lungs during breathing. This explains why coughing often occurs in those who smoke cigarettes. The body's natural reaction is to increase mucus production. In addition, mucus aids in moisturizing the inhaled air and prevents tissues such as the nasal and airway epithelia from drying out.[4] Nasal and airway mucus is produced continuously, with most of it swallowed subconsciously, even when it is dried.[5]
Increased mucus production in the respiratory tract is a symptom of many common illnesses, such as the common cold and influenza. Hypersecretion of mucus can occur in inflammatory respiratory diseases such as respiratory allergies, asthma, and chronic bronchitis.[4] The presence of mucus in the nose and throat is normal, but increased quantities can impede comfortable breathing and must be cleared by blowing the nose or expectorating phlegm from the throat.
Diseases involving mucus
[edit]In general, nasal mucus is clear and thin, serving to filter air during inhalation. During times of infection, mucus can change color to yellow or green either as a result of trapped bacteria[6] or due to the body's reaction to viral infection.[7] The green color of mucus comes from the heme group in the iron-containing enzyme myeloperoxidase secreted by white blood cells as a cytotoxic defense during a respiratory burst.
In the case of bacterial infection, the bacterium becomes trapped in already-clogged sinuses, breeding in the moist, nutrient-rich environment. Sinusitis is an uncomfortable condition which may include congestion of mucus. A bacterial infection in sinusitis will cause discolored mucus and would respond to antibiotic treatment; viral infections typically resolve without treatment.[8] Almost all sinusitis infections are viral and antibiotics are ineffective and not recommended for treating typical cases.[9]
In the case of a viral infection such as cold or flu, the first stage and also the last stage of the infection cause the production of a clear, thin mucus in the nose or back of the throat. As the body begins to react to the virus (generally one to three days), mucus thickens and may turn yellow or green. Viral infections cannot be treated with antibiotics, and are a major avenue for their misuse. Treatment is generally symptom-based; often it is sufficient to allow the immune system to fight off the virus over time.[10]
Upper respiratory tract
[edit]Increased mucus production in the upper respiratory tract is a symptom of many common ailments, such as the common cold. Nasal mucus may be removed by blowing the nose or by using nasal irrigation. Excess nasal mucus, as with a cold or allergies, due to vascular engorgement associated with vasodilation and increased capillary permeability caused by histamines,[11] may be treated cautiously with decongestant medications. Thickening of mucus as a "rebound" effect following overuse of decongestants may produce nasal or sinus drainage problems and circumstances that promote infection.
During cold, dry seasons, the mucus lining nasal passages tends to dry out, meaning that mucous membranes must work harder, producing more mucus to keep the cavity lined. As a result, the nasal cavity can fill up with mucus. At the same time, when air is exhaled, water vapor in breath condenses as the warm air meets the colder outside temperature near the nostrils. This causes an excess amount of water to build up inside nasal cavities. In these cases, the excess fluid usually spills out externally through the nostrils.[12]
Lower respiratory tract
[edit]Excess mucus production in the bronchi and bronchioles, as may occur in asthma, bronchitis or influenza, results from chronic airway inflammation, and hence may be treated with anti-inflammatory medications. Impaired mucociliary clearance due to conditions such as primary ciliary dyskinesia may also result in its accumulation in the bronchi.[3] The dysregulation of mucus homesotasis is the fundamental characteristic of cystic fibrosis, an inherited disease caused by mutations in the CFTR gene, which encodes a chloride channel. This defect leads to the altered electrolyte composition of mucus, which triggers its hyperabsorption and dehydration. Such low-volume, viscous, acidic mucus causes has a reduced antimicrobial function, which facilitates bacterial colonisation.[13] The thinning of the mucus layer ultimately affects the PCL, which becomes dehydrated, compromising ciliary function and impairing mucociliary clearance.[3][13]
Digestive system
[edit]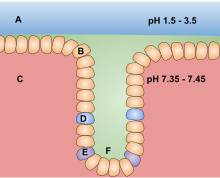
In the human digestive system, mucus is used as a lubricant for materials that must pass over membranes, e.g., food passing down the esophagus. Mucus is extremely important in the intestinal tract. It forms an essential layer in the colon and in the small intestine that helps reduce intestinal inflammation by decreasing bacterial interaction with intestinal epithelial cells.[14] A layer of mucus along the inner walls of the stomach is vital to protect the cell linings of that organ from the highly acidic environment within it.[scientific 1] Mucus is not digested in the intestinal tract. Mucus is also secreted from glands within the rectum due to stimulation of the mucous membrane within. [citation needed]
Properties of mucus
[edit]Tunable Swelling Capacity
[edit]Mucus is able to absorb water or dehydrate through pH variations. The swelling capacity of mucus stems from the bottlebrush structure of mucin within which hydrophilic segments provide a large surface area for water absorption. Moreover, the tunability of swelling effect is controlled by polyelectrolyte effect.
Polyelectrolyte Effect in Mucus
[edit]Polymers with charged molecules are called polyelectrolytes. Mucins, a kind of polyelectrolyte proteoglycans, are the main component of mucus, which provides the polyelectrolyte effect in mucus.[15] The process of inducing this effect comprises two steps: attraction of counter-ions and water compensation. When exposed in physiological ionic solution, the charged groups in the polyelectrolytes attract counter-ions with opposite charges, thereby leading to a solute concentration gradient. An osmotic pressure is introduced to equalize the concentration of solute throughout the system by driving water to flow from the low concentration areas to the high concentration areas. In short, the influx and outflux of water within mucus, managed by the polyelectrolyte effect, contribute to mucus' tunable swelling capacity[16].
Mechanism of pH-Tunable Swelling
[edit]The ionic charges of mucin are mainly provided by acidic amino acids including aspartic acids (pKa=3.9) and glutamic acids (pKa=4.2). The charges of acidic amino acids will change with environmental pH value due to acid dissociation and association. Aspartic acid, for example, has a negative side chain when the pH value is above 3.9, while a neutrally charged side chain will be introduced as pH value drops below 3.9. Thus, the number of negative charges in mucus is influenced by the pH value of surrounding environment. That is, the polyelectrolyte effect of mucus is largely affected by the pH value of solution due to the charge variation of acidic amino acid residues on the mucin backbone. For instance, the charged residue on mucin is protonated at a normal pH value of the stomach, approximately pH 2. In this case, there is scarcely polyelectrolyte effect, thereby causing compact mucus with little swelling capacity. However, a kind of bacteria, Helicobacter pylori, is prone to producing base to elevate the pH value in stomach, leading to the deprotonation of aspartic acids and glutamic acids, i.e., from neutral to negative-charged. The negative charges in the mucus greatly increase, thus inducing the polyeletrolyte effect and the swelling of the mucus. This swelling effect increases the pore size of the mucus and decreases mucus' viscosity, which allows bacteria to penetrate and migrate into the mucus and cause disease. [17]
Charge Selectivity
[edit]The high selective permeability of mucus plays a crucial role in the healthy state of human beings by limiting the penetration of molecules, nutrients, pathogens, and drugs. The charge distribution within mucus serves as a charge selective diffusion barrier, thus significantly affecting the transportation of agents. Among particles with various surface zeta potentials, cationic particles tend to have a low depth of penetration, neutral ones possess medium penetration, and anionic ones have the largest penetration depth. Furthermore, the effect of charge selectivity changes when the status of the mucus varies, i.e., native mucus has a threefold higher potential to limit agent penetration than purified mucus.[18].
See also
[edit]- ^ "What's a Booger?". KidsHealth.
- ^ Lillehoj, ER; Kim, KC (December 2002). "Airway mucus: its components and function". Archives of Pharmacal Research. 25 (6): 770–80. PMID 12510824.
- ^ a b c Mall, MA (March 2008). "Role of Cilia, Mucus, and Airway Surface Liquid in Mucociliary Dysfunction: Lessons from Mouse Models". Journal of Aerosol Medicine and Pulmonary Drug Delivery. 21 (1): 13–24. doi:10.1089/jamp.2007.0659.
- ^ a b Thorton, DJ; Rousseau, K; MucGuckin, MA (2008). "Structure and function of the polymeric mucins in airways mucus". Annual Review of Physiology. 70 (44): 459–486. doi:10.1146/annurev.physiol.70.113006.100702. PMID 17850213.
- ^ Gates, Stefan (2006). "Boogers". Gastronaut: Adventures in Food for the Romantic, the Foolhardy, and the Brave. pp. 68, 69. ISBN 0-15-603097-7.
- ^ "Runny Nose (with green or yellow mucus)". Get Smart: Know When Antibiotics Work. Centers for Disease Control and Prevention. March 9, 2006. Archived from the original on Mar 8, 2008.
- ^ "Yellow-green Phlegm and Other Myths". University of Arizona campus health services. Retrieved 2007-10-22.
- ^ Consumer Reports; American Academy of Family Physicians (April 2012), "Treating sinusitis: Don't rush to antibiotics" (PDF), Choosing Wisely: an initiative of the ABIM Foundation, Consumer Reports, retrieved August 17, 2012
- ^ American Academy of Family Physicians, "Five Things Physicians and Patients Should Question" (PDF), Choosing Wisely: an initiative of the ABIM Foundation, presented by ABIM Foundation, American Academy of Family Physicians, retrieved August 14, 2012
- ^ "Definition of Viral Infection". MedicineNet.com. Retrieved 2010-04-04.
- ^ Monroe EW, Daly AF, Shalhoub RF (February 1997). "Appraisal of the validity of histamine-induced wheal and flare to predict the clinical efficacy of antihistamines". J. Allergy Clin. Immunol. 99 (2): S798–806. doi:10.1016/s0091-6749(97)70128-3. PMID 9042073.
- ^ "Why Does Cold Weather Cause Runny Noses?". NPR. Retrieved 2011-09-22.
- ^ a b Haq, Iram J; Gray, Michael A; Garnett, James P; Ward, Christopher; Brodlie, Malcolm (March 2016). "Airway surface liquid homeostasis in cystic fibrosis: pathophysiology and therapeutic targets". Thorax. 71 (3): 284–287. doi:10.1136/thoraxjnl-2015-207588.
- ^ Johansson, Malin E. V.; Gustafsson, Jenny K.; Sjöberg, Karolina E.; Petersson, Joel; Holm, Lena; Sjövall, Henrik; Hansson, Gunnar C. (2010-01-01). "Bacteria penetrate the inner mucus layer before inflammation in the dextran sulfate colitis model". PLoS One. 5 (8): e12238. doi:10.1371/journal.pone.0012238. ISSN 1932-6203. PMC 2923597. PMID 20805871.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Sircar, S.; Keener, J. P.; Fogelson, A. L. (2013-01-07). "The effect of divalent vs. monovalent ions on the swelling of Mucin-like polyelectrolyte gels: Governing equations and equilibrium analysis". The Journal of Chemical Physics. 138 (1): 014901. doi:10.1063/1.4772405. ISSN 0021-9606.
- ^ Harding, S. E.; Creeth, J. M. (1983-07-28). "Polyelectrolyte behaviour in mucus glycoproteins". Biochimica Et Biophysica Acta. 746 (1–2): 114–119. ISSN 0006-3002. PMID 6871229.
- ^ Celli, Jonathan P.; Turner, Bradley S.; Afdhal, Nezam H.; Keates, Sarah; Ghiran, Ionita; Kelly, Ciaran P.; Ewoldt, Randy H.; McKinley, Gareth H.; So, Peter (2009-08-25). "Helicobacter pylori moves through mucus by reducing mucin viscoelasticity". Proceedings of the National Academy of Sciences. 106 (34): 14321–14326. doi:10.1073/pnas.0903438106. ISSN 0027-8424. PMID 19706518.
- ^ Crater, Jason S.; Carrier, Rebecca L. (2010-12-08). "Barrier Properties of Gastrointestinal Mucus to Nanoparticle Transport". Macromolecular Bioscience. 10 (12): 1473–1483. doi:10.1002/mabi.201000137. ISSN 1616-5195.
Cite error: There are <ref group=scientific> tags on this page, but the references will not show without a {{reflist|group=scientific}} template (see the help page).
