User:Mr. Ibrahem/AV nodal reentrant tachycardia
| AV-nodal reentrant tachycardia | |
|---|---|
| Other names | Atrioventricular nodal reentrant tachycardia, atrioventricular nodal reentry tachycardia |
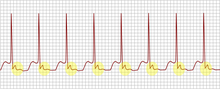 | |
| ECG tracing of typical AV nodal reentrant tachycardia. Highlighted in yellow is the P wave that falls after the QRS complex. | |
| Specialty | Cardiology |
| Symptoms | Palpitations, neck pounding, lightheadedness, shortness of breath, chest discomfort[1][2] |
| Usual onset | Sudden[3] |
| Duration | Episodic[4] |
| Types | Slow-fast, fast-slow, slow-slow[1] |
| Diagnostic method | Electrocardiogram (ECG), electrophysiology studies[1][5] |
| Differential diagnosis | Atrioventricular reentrant tachycardia, focal atrial tachycardia, junctional ectopic tachycardia, atrial flutter[1] |
| Treatment | Vagal maneuvers, adenosine, electrical cardioversion, ablation[1] |
| Prognosis | Generally good[1] |
AV-nodal reentrant tachycardia (AVNRT) is a type of abnormal fast heart rhythm.[6] Symptom may include episodes of palpitations, neck pounding, lightheadedness, shortness of breath, increased urination, and chest discomfort.[1][4][2] Onset is generally sudden.[3] Complications may include a heart attack in those with preexisting coronary artery disease.[1]
It is generally not associated with underlying heart disease.[1] The underlying mechanism is believed to involve two pathways in the atrioventricular (AV) node that conduct at different speeds.[3] Diagnosis is supported by an electrocardiogram (ECG) showing a regular heart rate of 140 to 280 beats per minute and a narrow QRS complex.[1] The P waves are generally not visible as they occur within the QRS complex.[3]
Treatment is with specific physical maneuvers, medications, or electrical cardioversion.[1] Medications used may include adenosine or diltiazem.[1] The initial recommended dose for cardioversion is 50 to 100J.[3] Frequent attacks may be treated with radiofrequency ablation.[1] If this is not an option beta blockers or diltiazem may be used long term.[2] Outcomes are generally good.[1]
AV nodal reentrant tachycardia represents about 60% of cases of paroxysmal supraventricular tachycardia (SVT).[1] Onset is most often in people between 14 to 50 years old.[2] Women are affected twice as often as men.[3] The underlying mechanism was first descripted in 1973 by Denes.[5]
References[edit]
- ^ a b c d e f g h i j k l m n o Hafeez, Y; Armstrong, TJ (January 2020). "Atrioventricular Nodal Reentry Tachycardia". PMID 29763111.
{{cite journal}}: Cite journal requires|journal=(help) - ^ a b c d Page, Richard L.; Joglar, José A.; Caldwell, Mary A.; Calkins, Hugh; Conti, Jamie B.; Deal, Barbara J.; Estes, N. A. Mark; Field, Michael E.; Goldberger, Zachary D. (May 2016). "2015 ACC/AHA/HRS Guideline for the Management of Adult Patients With Supraventricular Tachycardia: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society". Journal of the American College of Cardiology. 67 (13): e27–e115. doi:10.1016/j.jacc.2015.08.856. ISSN 1558-3597. PMID 26409259.
- ^ a b c d e f Helton, MR (1 November 2015). "Diagnosis and Management of Common Types of Supraventricular Tachycardia". American family physician. 92 (9): 793–800. PMID 26554472.
- ^ a b Shenasa, Mohammad (2014). Electrocardiography of Complex Arrhythmias, An Issue of Cardiac Electrophysiology Clinics, E-Book. Elsevier Health Sciences. p. 483. ISBN 978-0-323-31210-3. Archived from the original on 2021-08-27. Retrieved 2021-02-09.
- ^ a b Katritsis, Demosthenes G; Camm, A. John (1 January 2006). "Classification and differential diagnosis of atrioventricular nodal re-entrant tachycardia". EP Europace. 8 (1): 29–36. doi:10.1093/europace/euj010.
- ^ Katritsis, Demosthenes G.; Camm, A. John (24 August 2010). "Atrioventricular Nodal Reentrant Tachycardia". Circulation. 122 (8): 831–840. doi:10.1161/CIRCULATIONAHA.110.936591.
