User:Posassium/sandbox
 | This is a user sandbox of Posassium. You can use it for testing or practicing edits. This is not the sandbox where you should draft your assigned article for a dashboard.wikiedu.org course. To find the right sandbox for your assignment, visit your Dashboard course page and follow the Sandbox Draft link for your assigned article in the My Articles section. |
Microglia to-do list[edit]
- Identify appropriate infobox (instead of blank anatomy infobox in article) ✓
- Add information to infobox (latin name, alternate names, antecedent cells, cytokines, stains, longevity, size)
- Add pictures to infobox (taken from article mainspace) ✓
- Improve readability of introduction paragraphs ✓
- Reorganize sections (put BBB info from intro into functions or purpose) and reconsider section titles (types→states, forms, or structure)
- Create a diagrams of different types of microglia
- Make new section for role in psychosis ✓
- Add see also section and find pages to link to ✓
This article relies excessively on references to primary sources. |
Microglia[edit]
 Microglia in resting state from rat cortex before traumatic brain injury (lectin staining with HRP) | |
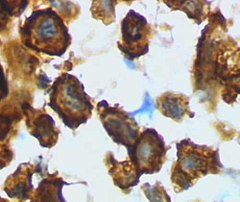 Microglia in activated form from rat cortex after traumatic brain injury (lectin staining with HRP) | |
| Alternate Names | Microgliocyte, Gitter cell, Hortega Cell |
|---|---|
| Embryological Origin | Yolk-sac derived erythromyeloid progenitors |
| Antecedent Cell(s) | Hematopoietic stem cells, monocytes |
| System | Central nervous system |
| Location(s) | Brain and spinal cord |
| Longevitiy | Up to lifetime of organism[1] |
| Function(s) | Immune regulation, synaptic and neuronal pruning, extracellular signaling |
| Cytokine(s) | IFN-γ, IL-1α, IL-1β, IL-6,[2] IL-8, IL-18,[3] TNF-α[2] |
| Stains | CD68, Iba1, lectin proteins GS-1, RCA, WGA, and ConA,[4] LN3, TSPO[5] |
| FMA | 54539 |
| NeuroLexID | sao789292116 |
| DorlandsID | 100066351 |
Microglia are a type of glial cell located throughout the brain and spinal cord.[6] Microglia account for 10–15% of all cells found within the brain.[7] As the resident macrophage cells, they act as the first and main form of active immune defense in the central nervous system (CNS).[8] Microglia (and other glia including astrocytes) are distributed in large non-overlapping regions throughout the CNS.[9][10] Microglia are key cells in overall brain maintenance — they are constantly scavenging the CNS for plaques, damaged or unnecessary neurons and synapses, and infectious agents.[11] Since these processes must be efficient to prevent potentially fatal damage, microglia are extremely sensitive to even small pathological changes in the CNS.[12] This sensitivity is achieved in part by the presence of unique potassium channels that respond to even small changes in extracellular potassium.[11]
Microglia directly interact with both pathogens and with neurons. [8]
Microglia can adopt one of several forms depending on signals detected from both inside and outside the cell.[13] These cells monitor the CNS and may change their form under episodic conditions (e.g. illness, injury etc.) or persistent conditions (e.g. development and aging, psychiatric and neurodegenerative disease, autoimmune disorders, and other immune stressors).[14] To accomplish their role in improving the overall health of the brain, microglia upregulate or downregulate the expression of many cytokines and other molecules that can have profound impacts on nearby neurons.[13][8]
Microglia that are in resting state provide structural support to nearby neurons and regulate the chemical environment.
Origin[edit]
Text from live article omitted — but it needs a lot of work.
History[edit]
Omitted
Types → rename to forms[edit]
Microglial cells are extremely plastic, and undergo a variety of structural changes based on location and system needs. This level of plasticity is required to fulfill the vast variety of functions that microglia perform. The ability to transform distinguishes microglia from macrophages, which must be replaced on a regular basis, and provides them the ability to defend the CNS on extremely short notice without causing immunological disturbance.[11]
Ramified[edit]
This form of microglial cell is commonly found at specific locations throughout the entire brain and spinal cord in the absence of foreign material or dying cells. This "resting" form of microglia is composed of long branching processes and a small cellular body. Unlike the ameboid forms of microglia, the cell body of the ramified form remains fairly motionless, while its branches are constantly moving and surveying the surrounding area. The branches are very sensitive to small changes in physiological condition and require very specific culture conditions to observe in vitro. Unlike activated or ameboid microglia, ramified microglia are unable to phagocytose cells and display little or no immunomolecules. This includes the MHC class I/II proteins normally used by macrophages and dendritic cells to present antigens to t-cells, and as a result ramified microglia function extremely poorly as antigen presenters. The purpose of this state is to maintain a constant level of available microglia to detect and fight infection, while maintaining an immunologically silent environment.[15][16]
Amoeboid[edit]
This form of microglial cell is found mainly within the perinatal white matter areas in the corpus callosum known as the "Fountains of Microglia." This shape allows the microglial free movement throughout the neural tissue, which allows it to fulfill its role as a scavenger cell. Amoeboid microglia are able to phagocytose debris, but do not fulfill the same antigen-presenting and inflammatory roles as activated microglia. Amoeboid microglia are especially prevalent during the development and rewiring of the brain, when there are large amounts of extracellular debris and apoptotic cells to remove.[11][17][16]
Activated[edit]
Microglia may become activated in the presence of direct immune threats, which occurs when pathogens cross the protective endothelial cells of the blood-brain barrier (or BBB) which normally prevents most pathogens from reaching vulnerable nervous tissue. As few antibodies are small enough to cross the BBB, microglia are responsible for recognizing and acting on immune threats. In actively defending the CNS from immune challenges, they may also swallow foreign bodies, act as antigen-presenting cells, activate T-cells, and induce or reduce inflammation.[12] Microglia may also become activated in order to rid the brain of unhealthy or unnecessary synapses and neurons. [[[moved/edited from introduction]]] Rest of section omitted
Gitter cells[edit]
Omitted
Perivascular[edit]
Omitted
Juxtavascular[edit]
Omitted
Functions[edit]

Microglial cells fulfill a variety of different tasks within the CNS mainly related to both immune response and maintaining homeostasis. The following are some of the major known functions carried out by these cells.
Scavenging[edit]
Omitted
Phagocytosis[edit]
One of the primary roles of microglia, phagocytosis, involves the engulfing of various materials. Engulfed materials generally consist of cellular debris, lipids, and apoptotic cells in the non-inflamed state, and invading virus, bacteria, or other foreign materials in the inflamed state. Once the microglial cell is "full" it stops phagocytic activity and changes into a relatively non-reactive gitter cell.
Cytotoxicity[edit]
Omitted
Antigen presentation[edit]
Omitted
Synaptic stripping[edit]
Omitted but this needs so much more info! THIS ARTICLE DOESN'T ACKNOWLEDGE MICROGLIA AS PERPETUATORS OF NEURONAL DEVELOPMENT!
Promotion of repair[edit]
Omitted
Extracellular signaling[edit]
Omitted
Role in psychosis[edit]
Microglial-induced neuroinflammation is a characteristic symptom of psychosis.[14] Under immune stress, the release of pro-inflammatory cytokines is upregulated and contributes to excessive inflammatory conditions.[18]
Schizophrenia[edit]
Immune stressors (including direct injury, emotional trauma, significant hormonal events, disease, and others) and genetic predispositions can dysregulate normal microglial functioning and contribute to the development of schizophrenia.[19] Microglia in the brains of people with schizophrenia are chronically overactive, contributing to lower overall CNS volume and impaired neuron connectivity.[14] Microgliosis, or a pervasive and persistent activation of microglia, has been seen in clinical trials and animal models particularly in the frontal and temporal cortices.[20]
Microglial secretion of pro-inflammatory cytokines is upregulated both during disease development and after onset. The gene locus most strongly associated with schizophrenia, the major histocompatibility complex locus, is directly relevant to microglial production of C4 proteins and regulation of neuroinflammation.[21]
See also[edit]
Notes[edit]
- ^ Prinz, Marco; Tay, Tuan Leng; Wolf, Yochai; Jung, Steffen (21 March 2014). "Microglia: unique and common features with other tissue macrophages". Acta Neuropathologica. 128 (3): 319–331. doi:10.1007/s00401-014-1267-1. PMID 24652058.
- ^ a b Shattuck, Eric C.; Muehlenbein, Michael P. (May 2015). "Human sickness behavior: Ultimate and proximate explanations". American Journal of Physical Anthropology. 157 (1): 1–18. doi:10.1002/ajpa.22698.
- ^ Alboni, Silvia; Cervia, Davide; Sugama, Shuei; Conti, Bruno (2010). "Interleukin 18 in the CNS". Journal of Neuroinflammation. 7 (1): 9. doi:10.1186/1742-2094-7-9. PMID 10190688.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Colton, CA; Abel, C; Patchett, J; Keri, J; Yao, J (1992). "Lectin staining of cultured CNS microglia". The Journal of Histochemistry and Cytochemistry. 40 (4): 505–512. PMID 1372634.
- ^ Frick, L R; Williams, K; Pittenger, C (2013). "Microglial dysregulation in psychiatric disease". Clinical & Developmental Immunology. 2013. doi:10.1155/2013/608654.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Ginhoux, F; Lim, S; Low, D; Huber, T; Hoeffel, G (2013). "Origin and differentiation of microglia". Frontiers in Cellular Neuroscience. 7 (45). doi:10.3389/fncel.2013.00045. PMID 3627983.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Lawson L J, Perry V H, Gordon S (1992). "Turnover of resident microglia in the normal adult mouse brain". Neuroscience. 48: 405–415. doi:10.1016/0306-4522(92)90500-2.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b c Filiano, Anthony J.; Gadani, Sachin P.; Kipnis, Jonathan (August 2015). "Interactions of innate and adaptive immunity in brain development and function". Brain Research. 1617: 18–27. doi:10.1016/j.brainres.2014.07.050.
- ^ Kreutzberg GW (1995). "The First Line of Defense in Brain Pathologies". Drug Research. 45 (1): 357–360. PMID 7763326.
- ^ Bushong EA, Martone ME, Jones YZ, Ellisman MH (January 2002). "Protoplasmic astrocytes in CA1 stratum radiatum occupy separate anatomical domains". J. Neurosci. 22 (1): 183–92. PMID 11756501.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b c d Gehrmann J, Matsumoto Y, Kreutzberg GW (1995). "Microglia: intrinsic immuneffector cell of the brain". Brain Research Reviews. 20 (3): 269–287. doi:10.1016/0165-0173(94)00015-H. PMID 7550361.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Dissing-Olesen L, Ladeby L, Nielsen HH, Toft-Hansen H, Dalmau I, Finsen B (2007). "Axonal lesion-induced microglial proliferation and microglial cluster formation in the mouse". Neuroscience. 149 (1): 112–122. doi:10.1016/j.neuroscience.2007.06.037. PMID 17870248.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Perry, V. Hugh; Teeling, Jessica (4 June 2013). "Microglia and macrophages of the central nervous system: the contribution of microglia priming and systemic inflammation to chronic neurodegeneration". Seminars in Immunopathology. 35 (5): 601–612. doi:10.1007/s00281-013-0382-8.
- ^ a b c Bergink, Veerle; Gibney, Sinead; Drexhage, Hemmo (Oct 2014). "Autoimmunity, inflammation, and psychosis: a search for peripheral markers". Biological psychiatry. 75 (4). doi:10.1016/j.biopsych.2013.09.037.
{{cite journal}}:|access-date=requires|url=(help) - ^ Cite error: The named reference
Aloisi 2001was invoked but never defined (see the help page). - ^ a b Christensen RN, Ha BK, Sun F, Bresnahan JC, Michael SB. (2006). "Kainate Induces Rapid Redistribution of the Actin Cytoskeleton in Ameboid Microglia". Journal of Neuroscience Research. 84 (1): 170–181. doi:10.1002/jnr.20865. PMID 16625662.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Ferrer I, Bernet E, Soriano E, Del Rio T, Fonseca M (1990). "Naturally occurring cell death in the cerebral cortex of the rat and removal of dead cells by transitory phagocytes". Neuroscience. 39 (2): 451–458. doi:10.1016/0306-4522(90)90281-8. PMID 2087266.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Mizoguchi, Y; Kato, T A; Horikawa, H; Monji, A (2014). "Microglial intracellular Ca(2+) signaling as a target of antipsychotic actions for the treatment of schizophrenia". Frontiers in Cellular Neuroscience. 8 (370). doi:10.3389/fncel.2014.00370.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Frick, L R; Williams, K; Pittenger, C (2013). "Microglial dysregulation in psychiatric disease". Clinical & Developmental Immunology. 2013. doi:10.1155/2013/608654.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Garey, L (2010). "When cortical development goes wrong: schizophrenia as a neurodevelopmental disease of microcircuits". Journal of Anatomy. 217 (4).
- ^ Sekar, A; Bialas, A R; de Rivera, H; Davis, A; Hammond, T R; Kamitaki, N; et al. (2016). "Schizophrenia risk from complex variation of complement component 4". Nature. 530 (7589): 177–183. doi:10.1038/nature16549.
{{cite journal}}: Explicit use of et al. in:|last7=(help)
