User:Weiffenb/NOREPINEPHRINE TRANSPORTER DRAFT
The norepinephrine transporter (NET) is a monoamine transporter. It is responsible for the Na +/Cl --dependent reuptake of extracellular norepinephrine (NE). NET can also reuptake extracellular dopamine (DA). The reuptake of these two neurotransmitters is essential in regulating concentrations in the synaptic cleft. NETs, along with the other monoamine transporters, are the targets of many antidepressants and recreational drugs. In addition, a deficiency of NET is associated with many affective and autonomic disorders such as orthostatic intolerance and ADHD.[1][2] There is evidence that single-nucleotide polymorphisms in the NET gene (SLC6A2) may be an underlying factor in some of these disorders.[2]
Structure and Function[edit]
The norepinephrine transporter is composed of 12 transmembrane domains (TMDs). The intracellular portion contains an amino (NH
2-) group and carboxy (COOH-) group. In addition, there is a large extracellular loop located between TMD 3 and 4. [3] [4] [5] The protein is composed of 617 amino acids. [3]
NET functions to transport synaptically released norepinephrine back into the presynaptic neuron. As much as 90% of the norepinephrine released will be taken back up in the cell by NET. NET functions by coupling the influx of Na+ and Cl- with the transport of norepinephrine. This occurs at a fixed ratio of 1:1:1. [6] Both NET and DAT can transport norepinephrine and dopamine. The reuptake of norepinephrine and dopamine is essential in regulating the concentration of monoamine neurotransmitters in the synaptic cleft. The transporter also helps maintain homeostatic balances of the presynaptic neuron.[7]
Norepinephrine[edit]
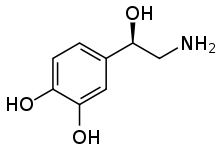
Norepinephrine (NE) is released from noradrenergic neurons that innervate both the CNS and PNS. NE, or noradrenaline (NA), has an important role in controlling mood, arousal, memory, learning, and pain perception. NE is a part of the sympathetic nervous system. [4] [8] Dysregulation of the removal of norepinephrine by NET is associated with many neuropsychiatric diseases. In addition, any antidepressants and recreational drugs compete for the binding of NET with NE. [3]
Transport Mechanisms[edit]
The transport of norepinephrine back into presynaptic cell is made possible by the cotransport with Na&2B and Cl%2B. The sequential binding of the ions results in the eventual reuptake of norepinephrine. The ion gradients of Na%2B and Cl%2B make this reuptake energetically favorable. The gradient is generated by the Na+/K+-ATPase which transports three sodium ions out and two potassium ions into the cell.[7] NETs have conductances similar to those of ligand gated ion channels. The expression of NET results in a leak-channel activity.[6] [7]
Location in the Nervous System[edit]
NETs are restricted to the noradrenergic neurons and are not present on neurons that release dopamine or epinephrine.[5] [4] [7] The transporters can be found along the cell body, axons, and dendrites of the neuron. [4] NETs are located away from the synapse, where norepinephrine is released, closer to the plasma membrane of the cell. This requires norepinephrine to diffuse from the site it is released to the transporter for reuptake.[7] Norepinephrine transporters are confined to the nerves of the sympathetic system, and those innervating the adrenal medulla, lung, and placenta. [7]
Regulation[edit]
Regulation of NET function is complex and a focus of current research. NETs are regulated at both the cellular and molecular level post-translation. The most understood mechanisms include phosphorylation by the second messenger protein kinase C (PKC). [5] PKC has been shown to inhibit NET function by sequestration of the transporter from the plasma membrane. [9] The amino acid sequence of NET has shown multiple sites related to protein kinase phosphorylation. [7] Post-translational modifications can have a wide range of effects on the function of the NET, including the rate of fusion of NET-containing vesicles with the plasma membrane, and transporter turnover. [9]
NET Gene[edit]
Gene Structure[edit]
The norepinephrine transporter gene, SLC6A2 is located on human chromosome 16 locus 16q12.2. This gene is encoded by 14 exons.[2] Based on the nucleotide and amino acid sequence, the NET transporter consists of 617 amino acids with 12 membrane-spanning domains. The structural organization of NET is highly homologous to other members of a sodium/chloride-dependent family of neurotransmitter transporters, including dopamine, epinephrine, serotonin and GABA transporters.[2]
Single Nucleotide Polymorphisms (SNPs)[edit]
A single-nucleotide polymorphism (SNP) is a genetic variation in which a genome sequence is altered by a single nucleotide (A, T, C or G). Coding single nucleotide polymorphisms (cSNPs) can be nonsynonymous, which alters the amino acid sequence, or synonymous, which would not change the resulting amino acid sequence. Nonsynonymous cSNPs have the potential to alter protein structure and function. NET proteins with an altered amino acid sequence (a missense mutation) could potentially be associated with various diseases that involve abnormally high or low plasma levels of norepinephrine due to altered NET function. NET SNPs and possible associations with various diseases are an area of focus for many research projects. There is evidence suggesting a relationship between NET SNPs and various disorders such as ADHD [10][2] psychiatric disorders, [2] postural tachycardia [2][11] and orthostatic intolerance.[2][11] The SNPs rs3785143 and rs11568324 have been related to attention-deficit hyperactivity disorder.[12] Thus far, however, the only confirmed direct association between a SNP and a clinical condition is that of the SNP, Ala457Pro, and orthostatic intolerance.[2] Thirteen NET missense mutations have been discovered so far.[2]
| Location | Amino Acid Variant | Related Disease |
|---|---|---|
| Exon 2 | Val69Ile | None |
| Exon 3 | Thr99Ile | None |
| Exon 5 | Val245Ile | None |
| Exon 6 | Asn292Thr | None |
| Exon 8 | Val356Leu | None |
| Exon 8 | Ala369Pro | None |
| Exon 8 | Asn375Ser | None |
| Exon 10 | Val449Ile | None |
| Exon 10 | Ala457Pro | Orthostatic intolerance |
| Exon 10 | Lys463Arg | None |
| Exon 11 | Gly478Ser | None |
| Exon 12 | Phe528Cys | None |
| Exon 13 | Tyr548His | None |
Additional Genetic Variations[edit]
An epigenetic mechanism (hypermethylation of CpG islands in the NET gene promoter region) that results in reduced expression of the noradrenaline transporter and consequently a phenotype of impaired neuronal reuptake of norepinephrine has been implicated in both postural orthostatic tachycardia syndrome and panic disorder.[14]
Clinical Significance[edit]
Orthostatic Intolerance[edit]
Orthostatic intolerance (OI) is a disorder of the autonomic nervous system (a subcategory of dysautonomia) characterized by the onset of symptoms upon standing. Symptoms include fatigue, lightheadedness, headache, weakness, increased heart rate/heart palpitations, anxiety, and altered vision.[2] Oftentimes, patients have high plasma norepinephrine (NE) concentrations (at least 600 pg/ml) in relation to sympathetic outflow upon standing, suggesting OI is a hyperadrenergic condition.[2][11] The discovery of identical twin sisters both suffering from OI suggested a genetic basis for the disorder.[2][11] A missense mutation on the NET gene (SLC62A) was discovered in which an alanine residue was replaced with a proline residue (Ala457Pro) in a highly conserved region of the transporter.[2] The patients’ defective NET had only 2% of the activity of the wild-type version of the gene.[2] The genetic defect in the NET protein results in decreased NET activity that could account for abnormally high NE plasma levels in OI. However, 40 other OI patients did not have the same missense mutation, indicating other factors contributed to the phenotype in the identical twins.[2] This discovery of the linkage with NET mutations that results in decreased activity and orthostatic intolerance suggests faulty NE uptake mechanisms can contribute to cardiovascular disease.[15]
Therapeutic Potential[edit]
"The involvement of the norepinephrine transporter (NET) in the pathophysiology and treatment of attention deficit hyperactivity disorder (ADHD), substance abuse, neurodegenerative disorders (e.g., Alzheimer's disease (AD) and Parkinson's disease (PD)) and clinical depression has long been recognized. [2006]"[16]
Depression[edit]


Certain antidepressant medications act to raise noradrenaline, such as serotonin-norepinephrine reuptake inhibitors (SNRIs), norepinephrine-dopamine reuptake inhibitors (NDRIs), norepinephrine reuptake inhibitors (NRIs or NERIs) and the tricyclic antidepressants (TCAs). These medications prevent NET from functioning normally, resulting in higher extracellular concentrations of NE. Noradrenaline therefore remains in the synapse longer, allowing it to reach more normal levels. Since the noradrenaline transporter is responsible for most of the dopamine clearance in the prefrontal cortex,[17] SNRIs would also raise dopamine levels in synapses there. However, dopamine in most brain regions is cleared primarily by the dopamine transporter, which works roughly ten times faster.[18] For many years, the number one choice in treating mood disorders like depression was through the uptake of TCAs, such as desipramine (Norpramin), nortriptyline (Arentyl, Pamelor), protriptyline (Vivactil) and amoxapine (Asendin).[19] However, currently far more potent drugs have been developed in the US, most notably the discovery of selective serotonin reuptake inhibitors (SSRIs). SSRIs affect the communication between chemical messengers in the brain by regulating how much of a certain chemical messenger enters the brain.[19] SSRIs regulate serotonin levels in the brain, which seems to aid the brain in exchanging messages more efficiently and in turn livens mood.[20] Drugs such as fluoxetine and paroxetine are both very impelling in treating mood disorders because they reduce many of the side effects one receives compared to using TCAs to treat such mood disorders.[20]
ADHD[edit]

The strong NET inhibitor atomoxetine (Strattera) has been approved by the FDA to treat ADHD in adults. [21][22] It works to increase the one's ability to focus, decrease any impulsiveness, and lessen hyperactivity in both children and adults who suffer from ADHD. [23] It is the first ADHD drug to be developed that reduces any risk of substance abuse for patients who continually take atomoxetine for their ADHD. The FDA approved another drug called Vyvanse specifically prescribed to children between the ages of 6 and 12 to treat ADHD. Both drugs for adults and children had common side effects similar to decreased appetite, bad sleeping habits, stomachaches and headaches.[21] Other common drugs that have been previously prescribed to treat ADHD in adults and children include Methylphenidate (Ritalin, Metadate, Concerta, Daytrana), Amphetamine (Adderall) and Dextroamphetamine (Dexadrine, Detrostat). [21]
Schizophrenia[edit]

The role of NE in schizophrenia has not been fully understood, but has stimulated research into this topic. [24] The only relationship that has been understood between researchers is that there is a positive correlation between increased NE levels in the brain and activity of schizophrenia.[24] Before the age of modern treatment of schizophrenia, patients that were mentally ill were not treated and instead that were hidden away in their homes.[24] Old treatments often included sedatives, electroconvulsive therapy (ECT), artificially induced comas and frontal lobotomies.[24] Unfortunately, the side effects of these treatments usually outweighed the therapeutic benefits of these treatments.[24] The first breakthrough for schizophrenia treatment was the discovery of the antipsychotic drug called Chlorpromazine (CPZ) in 1979, which is still in common use today.[24] Another drug developed from the class of atypical antipsychotic drug called Clozapine.[25] This drug works to help patients who have tried to injure/kill themselves before from getting no prior treatment. It works similarly to SSRIs by regulating the concentrations of certain chemical messengers in the brain.[25]
Psychostimulants[edit]
Cocaine[edit]
Cocaine is a powerful psychostimulant and known to be one of the best-known drugs of substance abuse.[26] Cocaine is a nonselective, competitive antagonist of norepinephrine, serotonin, and dopamine transport. This thwarts the absorption of these chemicals into the presynaptic terminal[26] and allows a large concentration of dopamine, serotonin and norepinephrine to build up in the cell. The potential for cocaine addiction is thought to be a result of its effects on dopamine transporters in the CNS, while it has been suggested that the life-threatening cardiovascular effects of cocaine may involve the inhibition of NETs at sympathetic and CNS autonomic synapses. [27]
Amphetamines[edit]

Amphetamines have a similar effect on norepinephrine levels compared to that of cocaine in that increases NE levels in the brain.[28] Amphetamine-like drugs are substrates for monoamine transporters, include NET, that cause a reversal in the direction of neurotransmitter transport.[7][29] Amphetamines cause a large accumulation of extracellular NE.[28] High levels of NE in the brain account for most of the profound effects of amphetamines, including alertness, anorectic, locomotor and sympathomimetic effects.[28] However, the effects that amphetamines have on the brain are slower but last longer than the effects cocaine has on the brain.[28] MDMA (3,4-Methylenedioxymethamphetamine or "ecstacy") is an amphetamine with wide recreational use. A study reported that the NET inhibitor Reboxetine reduced the stimulant effects of MDMA in humans, demonstrating the crucial role NET has in the cardiovascular and stimulant-like effects of MDMA.[30]
Further Research[edit]
NETs role in many brain disorders underlies the importance of understanding the (dys)regulation of the transporter. A complete model of the proteins that associate with the transporter will be useful in designing drug therapies for diseases such as schizophrenia, affective disorder, and autonomic disorders. Recently discovered mechanisms of the NET, including the ability to act reversibly and as an ion channel, provide other areas of research. [7] [5]
See also[edit]
- Neurotransmitter transporter
- Sodium:neurotransmitter symporter
- Solute carrier family
- Norepinephrine
- Monoamine transporter
- Orthostatic intolerance
- Single-nucleotide polymorphisms
References[edit]
- ^ S. Schroeter, S. Apparsundaram, R. G. Wiley, L. H. Miner, S. R. Sesack & R. D. Blakely (May 2000). "Immunolocalization of the cocaine- and antidepressant-sensitive l-norepinephrine transporter". The Journal of Comparative Neurology. 420 (2): 211–232. doi:10.1002/(SICI)1096-9861(20000501)420:2<211::AID-CNE5>3.0.CO;2-3. PMID 10753308.
{{cite journal}}: CS1 maint: date and year (link) CS1 maint: multiple names: authors list (link) - ^ a b c d e f g h i j k l m n o p q Tellioglu T, Robertson D (November 2001). "Genetic or acquired deficits in the norepinephrine transporter: current understanding of clinical implications" (PDF). Expert Rev Mol Med. 2001 (29): 1–10. doi:10.1017/S1462399401003878. PMID 14987367.
{{cite journal}}: CS1 maint: date and year (link) - ^ a b c Stöber, Gerald; Nöthen, Markus M.; Pörzgen, Peter; Brüss, Michael; Bönisch, Heinz; Knapp, Michael; Beckmann, Helmut; Propping, Peter (NaN undefined NaN). "Systematic search for variation in the human norepinephrine transporter gene: Identification of five naturally occurring missense mutations and study of association with major psychiatric disorders". American Journal of Medical Genetics. 67 (6): 523–532. doi:10.1002/(SICI)1096-8628(19961122)67:6<523::AID-AJMG3>3.0.CO;2-I. PMID 8950409.
{{cite journal}}: Check date values in:|date=(help) - ^ a b c d Schroeter, S.; Apparsundaram, S.; Wiley, R. G.; Miner, L. H.; Sesack, S. R.; Blakely, R. D. (2000 May 1). "Immunolocalization of the cocaine- and antidepressant-sensitive l-norepinephrine transporter". The Journal of Comparative Neurology. 420 (2): 211–32. doi:10.1002/(SICI)1096-9861(20000501)420:2<211::AID-CNE5>3.0.CO;2-3. PMID 10753308.
{{cite journal}}: Check date values in:|date=(help) - ^ a b c d Sager, J. J.; Torres, G. E. (2011 Aug 30). "Proteins interacting with monoamine transporters: current state and future challenges". Biochemistry. 50 (34): 7295–310. doi:10.1021/bi200405c. PMID 21797260.
{{cite journal}}: Check date values in:|date=(help) - ^ a b Galli, A.; Defelice, L. J.; Duke, B. J.; Moore, K. R.; Blakely, R. D. (1995 Oct). "Sodium-dependent norepinephrine-induced currents in norepinephrine-transporter-transfected HEK-293 cells blocked by cocaine and antidepressants". The Journal of Experimental Biology. 198 (Pt 10): 2197–212. doi:10.1242/jeb.198.10.2197. PMID 7500004.
{{cite journal}}: Check date values in:|date=(help) - ^ a b c d e f g h i Torres, Gonzalo E.; Gainetdinov, Raul R.; Caron, Marc G. (NaN undefined NaN). "Plasma membrane monoamine transporters: structure, regulation and function". Nature Reviews Neuroscience. 4 (1): 13–25. doi:10.1038/nrn1008. PMID 12511858.
{{cite journal}}: Check date values in:|date=(help) - ^ Zhou, J (2004 Dec). "Norepinephrine transporter inhibitors and their therapeutic potential". Drugs of the Future. 29 (12): 1235–1244. doi:10.1358/dof.2004.029.12.855246. PMC 1518795. PMID 16871320.
{{cite journal}}: Check date values in:|date=(help) - ^ a b Gether, U.; Andersen, P. H.; Larsson, O. M.; Schousboe, A. (2006 Jul). "Neurotransmitter transporters: molecular function of important drug targets". Trends in Pharmacological Sciences. 27 (7): 375–83. doi:10.1016/j.tips.2006.05.003. PMID 16762425.
{{cite journal}}: Check date values in:|date=(help) - ^ Kim CH, Hahn MK, Joung Y, Anderson SL, Steele AH, Mazei-Robinson MS, Gizer I, Teicher MH, Cohen BM, Robertson D, Waldman ID, Blakely RD, Kim KS (December 2006). "A polymorphism in the norepinephrine transporter gene alters promoter activity and is associated with attention-deficit hyperactivity disorder". Proc. Natl. Acad. Sci. U.S.A. 103 (50): 19164–9. doi:10.1073/pnas.0510836103. PMC 1748193. PMID 17146058.
{{cite journal}}: CS1 maint: date and year (link) CS1 maint: multiple names: authors list (link) - ^ a b c d Shannon JR, Flattem NL, Jordan J, Jacob G, Black BK, Biaggioni I, Blakely RD, Robertson D (February 2000). "Orthostatic intolerance and tachycardia associated with norepinephrine-transporter deficiency". N. Engl. J. Med. 342 (8): 541–9. doi:10.1056/NEJM200002243420803. PMID 10684912.
{{cite journal}}: CS1 maint: date and year (link) CS1 maint: multiple names: authors list (link) - ^ Kim JW, Biederman J, McGrath CL, Doyle AE, Mick E, Fagerness J, Purcell S, Smoller JW, Sklar P, Faraone SV (June 2008). "Further evidence of association between two NET single-nucleotide polymorphisms with ADHD". Mol. Psychiatry. 13 (6): 624–30. doi:10.1038/sj.mp.4002090. PMID 17876324.
{{cite journal}}: CS1 maint: date and year (link) CS1 maint: multiple names: authors list (link) - ^ Maarten E. A. Reith (2002). Neurotransmitter transporters: structure, function, and regulation. Humana Press. p. 120. ISBN 978-0-89603-945-2. Retrieved 27 October 2011.
- ^ Esler M, Alvarenga M, Pier C, Richards J, El-Osta A, Barton D, Haikerwal D, Kaye D, Schlaich M, Guo L, Jennings G, Socratous F, Lambert G (2006). "The neuronal noradrenaline transporter, anxiety and cardiovascular disease". J Psychopharmacol. 20 (4 Suppl): 60–6. doi:10.1177/1359786806066055. PMID 16785272.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Schroeder, Christoph; Tank, Jens; Boschmann, Michael; Diedrich, Andre; Sharma, Arya M.; Biaggioni, Italo; Luft, Friedrich C.; Jordan, Jens (2002), [Selective Norepinephrine Reuptake Inhibition as a Human Model of Orthostatic Intolerance "Selective Norepinephrine Reuptake Inhibition as a Human Model of Orthostatic Intolerance"], Circulation, 105 (3): 347–343, doi:10.1161/hc0302.102597, PMID 11804991, retrieved 2011-10-28
{{citation}}: Check|url=value (help) - ^ Information Hyperlinked Over Proteins (IHOP)
- ^ Morón JA, Brockington A, Wise RA, Rocha BA, Hope BT (January 2002). "Dopamine uptake through the norepinephrine transporter in brain regions with low levels of the dopamine transporter: evidence from knock-out mouse lines". J. Neurosci. 22 (2): 389–95. doi:10.1523/JNEUROSCI.22-02-00389.2002. PMC 6758674. PMID 11784783.
{{cite journal}}: CS1 maint: date and year (link) CS1 maint: multiple names: authors list (link) - ^ Yavich L, Forsberg MM, Karayiorgou M, Gogos JA, Männistö PT (September 2007). "Site-specific role of catechol-O-methyltransferase in dopamine overflow within prefrontal cortex and dorsal striatum". J. Neurosci. 27 (38): 10196–209. doi:10.1523/JNEUROSCI.0665-07.2007. PMC 6672678. PMID 17881525.
{{cite journal}}: CS1 maint: date and year (link) CS1 maint: multiple names: authors list (link) - ^ a b Zhou, Jia (December 2004). "Norepinephrine transporter inhibitors and their therapeutic potential". Drugs Future. 29 (12): 1235–1244. doi:10.1093/protein/5.5.455. PMC 1518795. PMID 1518795.
{{cite journal}}: CS1 maint: date and year (link) - ^ a b Mayo Clinic Staff, Selective serotonin reuptake inhibitors (SSRIs), retrieved 1 November 2011
- ^ a b c National Institutes of Mental Health, What medications are used to treat ADHD?, retrieved 2 November 2011
- ^ Dene Simpson & Greg L. Plosker (2004). "Atomoxetine: a review of its use in adults with attention deficit hyperactivity disorder". Drugs. 64 (2): 205–222. doi:10.2165/00003495-200464020-00005. PMID 14717619.
- ^ AHFS Consumer Medication Information, Atomoxetine, retrieved 2 November 2011
- ^ a b c d e f Decaire, Michael, The neurophysiology of schizophrenia: Etiology and Psychopharmacological treatment, retrieved 1 November 2011
- ^ a b AHFS Consumer Medication Information, Clozapine, retrieved 1 November 2011
- ^ a b Macey, Darrel (1 January 2003). "Chronic Cocaine Self-Administration Upregulates the Norepinephrine Transporter and Alters Functional Activity in the Bed Nucleus of the Stria Terminalis of the Rhesus Monkey". The Journal of Neuroscience. 23 (1): 12–16. doi:10.1523/JNEUROSCI.23-01-00012.2003. PMC 6742134. PMID 12514195.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Barker, Eric L. (2000). "http://www.acnp.org/g4/GN401000029/CH029.html". Psychopharmacology: The Fourth Generation of Progress. Retrieved 2011-11-02.
{{cite journal}}: External link in|title=|coauthors=ignored (|author=suggested) (help) - ^ a b c d Drug and Human Performance Fact Sheets, Methamphetamine (And Amphetamine), retrieved 1 November 2011
- ^ Sulzer, David (1995). "The Journal of Neuroscience" (PDF). Amphetamine Redistributes Dopamine from Synaptic Vesicles to the Cytosol and Promotes Reverse Transport. 15: 4102–4108. Retrieved 2011-11-02.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Hysek, C M (August 2011). "The Norepinephrine Transporter Inhibitor Reboxetine Reduces Stimulant Effects of MDMA ("Ecstasy") in Humans". Clinical Pharmacology & Therapeutics. 90 (2): 246–255. doi:10.1038/clpt.2011.78. PMID 21677639.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help)
